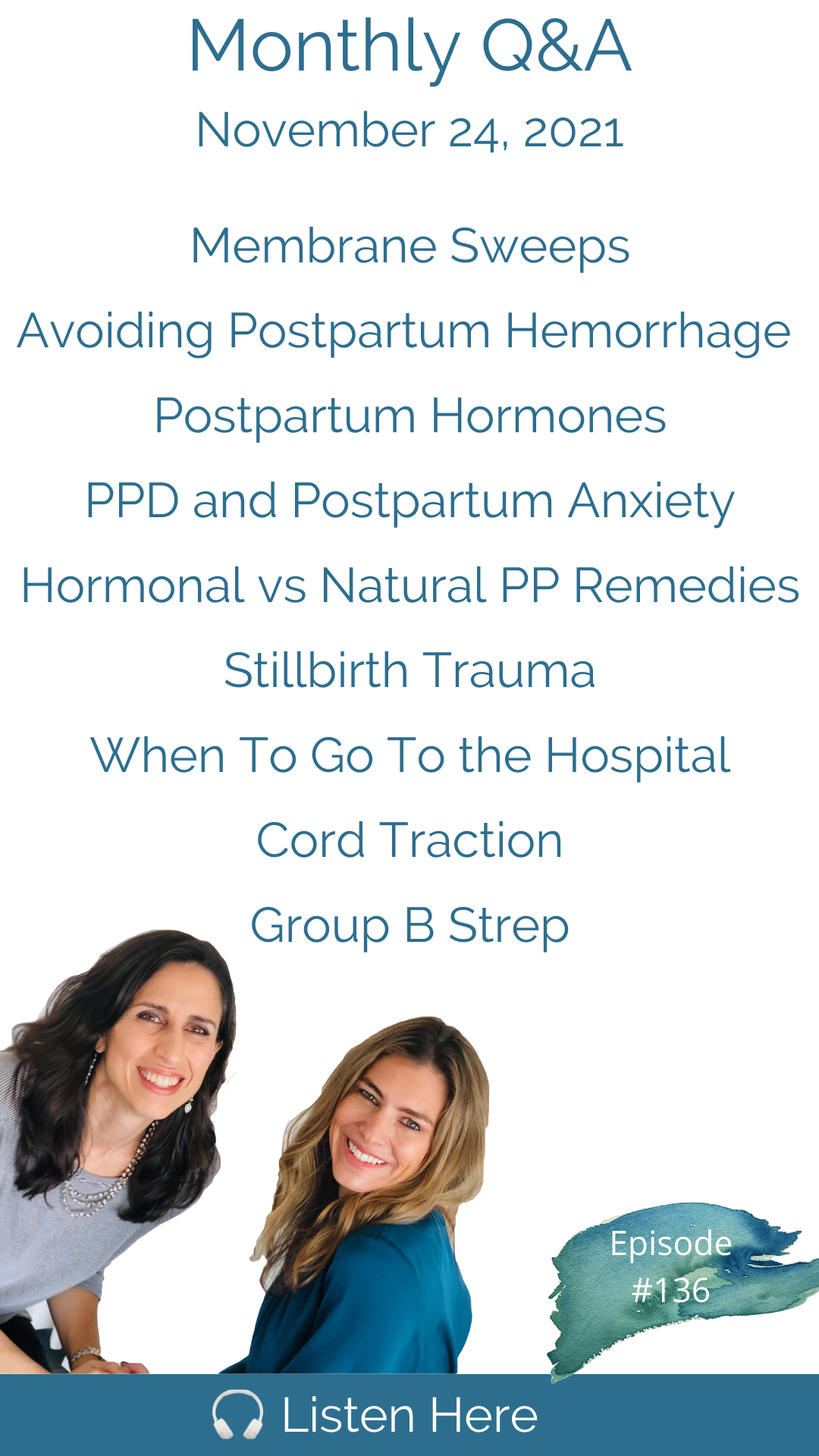
Our Q&A is here again! This month we had excellent questions from our community on whether or not you should have a membrane sweep in late pregnancy, how to avoid experiencing a postpartum hemorrhage, how and why postpartum hormones influence baby blues versus postpartum depression and anxiety; and whether there any hormonal treatments for postpartum mood disorders. How can one recover from the trauma of still birth; when should you go to the hospital in labor; and is cord traction necessary for birth of the placenta? And finally what to do if you test positive for Group B Strep and want a low-intervention birth. Thank you as always for your great questions and keep them coming! * * * * * * * * * * Connect with us on Instagram @DownToBirthShow, where we post new information daily related to pregnancy, childbirth and postpartum. You can reach us at Contact@DownToBirthShow.com. We are always happy to hear from our listeners and appreciate questions for our monthly Q&A episodes. To submit a question, visit the Down To Birth website or send us a voice memo through Instagram messenger. This show is sponsored by: Connect with Cynthia and Trisha at: Connect with Cynthia: Connect with Trisha at: Remember - we're in CT but you can be anywhere. We serve women and couples coast to coast with our live, online monthly HypnoBirthing classes, support groups and prenatal/postpartum workshops. We are so grateful for your reviews and shares - we love what we do and thank you all for your support! Please remember we don’t provide medical advice, and to speak with your licensed medical provider related to all your healthcare matters. Thanks so much for joining in the conversation, and see you next week! Support the show (https://www.paypal.com/paypalme/cynthiaovergard)
Postpartum Soothe*
Beautiful Births & Beyond*
*Use promo code DOWNTOBIRTH
You're in this really tough spot because you don't want to look controlling. You don't want to look like you're the more important parent, it's really hard.
What are you afraid of? If you wait too long, having the baby in the car, that doesn't happen very often, but if it happens, it usually works out okay? Going too soon is a much bigger problem.
Pitocin is the first thing that they give women in order to stop postpartum hemorrhage. It also can cause postpartum hemorrhage, if Pitocin is what in fact provider is going to kind of probably pinpoint you as already being a little bit.
Go ahead and say, Trisha, you know, you want to difficult, difficult. Oh, well.
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth
Hello, everyone, Trisha, you know how I want to start today, right? Tell me, I want to talk about that Instagram story that we posted where we asked our followers, what kind of provider you're seeing in your pregnancy, how long you spend in the waiting room, and how long you spend at your appointments on average. And I would say we got some pretty interesting responses. We got hundreds of responses in every category. And I think it told quite a bit of a story. Do you agree? Yeah, we did our own quick little research was excellent. It was quite telling. Were you surprised by the results? No. Yeah, it wasn't either. I was a little surprised. Should I go home birth midwife to OB or should I go the other way?
Let's go OB to home birth midwife.
So for for those of you with obstetricians, your average wait time is 31 minutes, your average visit time is 11 minutes. I think is worth pointing out that some people I looked I did the median times as well. And the there are a lot of people who were with their obstetricians five minutes, they would say their appointments for five minutes. Some said most of them said five to 10 minutes. One woman times hers and shared with us that she spent four minutes and 24 seconds with her doctor if you can believe that. But on average, waiting 31 minutes for an 11 minute appointment. That means you're spending 75% of your time in the waiting room.
For those sorry, but how did we get to an 11 minute average? There must have been some appointments with OBS that were actually lasting 25 minutes. Oh, yeah, a couple of women said 30 minutes, several said 20 to 25 minutes. Yeah, we had hundreds of responses in every category. And sure, yes, there was a minority of women at 20 something percent with sizable appointments that pulled up the averages dramatically. So one woman said she spent an hour with her OB so that affected the average, which is actually why I did the median. And the median appointment came in a couple minutes shorter. So I median would have been better data than averages but I still felt averages was a little more relatable, the median tells you the 50% mark so that came in at around nine minutes and change which means half of the responders spend under nine minutes at their appointment and half spend longer. So the averages get a little skewed by the anomalies, but it was so similar that I just want with the averages it really wasn't a big difference by minute or two. So the hospital based midwives are having women wait on average 11 minutes so again, some women say they walk right in so they get registered as zero minutes of wait time and others are waiting quite a long time but the average is for what it's worth is 11 minutes. The average appointment time is 25 minutes so a very quick improvement from waiting 31 minutes down to 11 minutes and from spending at the appointments 11 minutes with OBS all the way up to 25 minutes. It's very significant. Alright, birth center midwives waiting on average eight minutes again, a very large percentage of women said they walk right in some set. I've never even sat down in the waiting room but the average was eight minutes, the average appointment time 43 minutes. And of course who is going to come in with the best the best day to hear homebirth midwives over 70% of the women said they have no wait time some women said five to 10 minutes so the average came in at two minutes the average appointment time one hour and three minutes no see Trisha you're not surprised as a home birth midwife Are you know that's typically what you schedule an appointment for 60 minutes.
You don't intentionally as a way of life, keep them waiting.
No, we don't schedule. You know how that happens. You know how that happens? That would be it. scheduling one hour appointments every half an hour and counting on half your people not to show up. That's why it will be visits are tend to be that way. They're scheduled for maybe 15 to 20 minutes and they double book. Remember, they are, unfortunately profit driven. You know, it's a business model, it is the model. It's the model and that it's not that model in verse center or homebirth. Where is the hospital model isn't set up that way. It's it comes from a higher up place, many of these obese would love to practice that way. They would probably love to have 30 minute visits with all of their well, they went into the wrong line of work, then they should have become midwives. That's right. Even the male ones I'm not joking. Even the male ones can be midwives. Yeah, it's we know one that we had a male midwife in Connecticut. Remember? Oh, yeah, I do remember him? Yeah, it means with woman take. It still takes a confident man to say I'm a midwife, I'm sure but pretty awesome. Yeah, remember that? That Instagram follower shared with us that Mount Sinai in New York was featuring all their obstetric interns, and they were sharing like, Oh, they're trying to make them all relatable, like, show us a picture of you, with your dog and what you'd like to do on the weekend. And what's your favorite type of food? What's your favorite activity? And then they said, What made you want to become an obstetrician? And a majority of them wrote surgery, many of them childishly I think unprofessionally put an exclamation point after it surgery. Like, yay, surgery. Like, that's the part they're excited about. And then one had this beautiful response, like just to see the magic of birth with a mother and baby meeting for the first time. Yeah, thanks. Like, you're out there. But it wasn't the majority. So anyway, you know, all we ever say is you have to find the provider who is the right fit for you.
Period. Right. And you have to know what you're getting into. If you don't mind. A one of our, one of the responses to that question was five minutes, or her visit was like five to 10 minutes. And she was like, and that's exactly how I want it. I don't want to spend an hour with my midwife every week.
That's right. But I also want to say I'm certain that woman, whoever she is, also doesn't want to spend 31 minutes in the waiting room for those quick appointments either.
That's true. Nobody wants to waste their time. Yeah, so what we were really pointing out isn't only the duration of the appointments, but the relationship between the wait time and the appointment. So also, when you have long appointments with midwives, you're not captive, we usually they're chatting and building a relationship. And you don't have to stay that long. Usually, you want to usually you just want to form that relationship. Yeah, the the first 10 or 15 minutes is just catching up on life and family and things and it's not talking about your emotions. Yes, I have questions around birth. And then when you have a specific question related to where you are in that pregnancy, you get a thorough answer, not a one minute, or 32nd response. Right.
Which reminds me this is the last thing I have to say on the topic before we get into our questions, but one woman shared with me that at her obstetric appointments, and I believe she switched and provided data for her OB her OB and then for her midwife after switching, but she said her OB said to her you get three quick questions per visit.
The problem is that in care like that, even if they scheduled their visits for prenatal visits for 30 minutes, then in an eight hour workday, they can see 16 people and their bottom line needs them to see 30 Plus, and they will have 30 plus people on their schedule in a day. Sometimes 50, I don't think they deserve your business. Alright, bye. Ready to start? I'm ready. All right. The first one says, Trisha, what is your view on membrane sweeps? Hmm. So first, why don't you describe what that is?
Okay. So the membrane sweep is when your provider uses their fingers to go inside the cervix and create a separation between where the cervix and your amniotic sac connect. And it's it's actually a mechanical induction. It is a form of inducing labor, but it feels a lot more natural than, you know, Pitocin or some of the other things that we might do. So it tends to be kind of like first line, so using your fingers to separate the cervix from the amniotic sac. Releases prostaglandins and prostaglandins are the thing that gets you into labor. prostaglandins are also found in semen and that's one of the reasons that sex and late pregnancy and help bring on labor. So about a third of women choose to have a membrane membrane sweep. It does, as I said, Help ripen the cervix and start the labor. But it is uncomfortable, and it can if your body isn't ready, it can create false labor or can you create just uterine irritability? Which is no fun. So my view on it is that it's personal choice. The problem that comes up a lot with membrane sweeps is that it happens unintentionally, in quotes, when you get a cervical exam, oh, we're just going to check your cervix at your 39 or 40 week appointment, see how things are looking and you know why I'm in there, maybe I can just pull that cervix away from the the amniotic sac a little bit, you know, see if we can help get your labor going. That's a problem, right? Because a woman hasn't actually been informed of what's happening and doesn't understand that this is actually a form of induction, there is risk of breaking the bag of water. That's a serious risk factor. That was shown to happen in about 10% of cases.
It's often done, Trisha as the last resort before a chemical induction. Yeah, right. Now, like before we induce you with Pitocin. On Thursday, let's bring you in Wednesday, and we'll do a membrane sweep and send you home. Right. Yeah, that's why I sort of say it's like first line for when you're getting near induction. Or if you're trying to avoid a hospital based induction where you actually have to go in and have medication. I would totally say have a membrane sweep if or, you know, decline your induction if you don't want the membrane sweep, but I would choose this before other things for sure.
Okay, great. The next question is, are there any ways to avoid postpartum hemorrhage?
The number one reason that women have postpartum hemorrhage is uterine acne, which means the uterus is weak after birth and doesn't contract well. And one of the biggest contributors to uterine acne is overstimulation of the uterus that can happen through long labor for whatever reason, or Pitocin. So if you're really looking to prevent postpartum hemorrhage, I would say do your best to avoid Pitocin. There are other factors related to postpartum hemorrhage that we have a little less control over. Sometimes it's related to the way the placenta separates. We don't have a lot of control over that sometimes it's related to an overly stretched uterus, like twins obviously don't have a lot of control over that. Sometimes it can be related to blood clotting factors in your body.
And the question for you Pitocin is the first thing that they give women in order to stop postpartum hemorrhage. It also can cause postpartum hemorrhage, if Pitocin is what in fact caused the hemorrhage. Do they still give Pitocin to stop the hemorrhage? Or did they go to the other drugs now? Yeah, it's still Pitocin. And it actually does still work. It still works because it's a bolus of Pitocin, which makes the uterus quickly contract. But the thing is that prolonged Pitocin exposure over saturates the receptors, and then after birth, the uterus can be buggy, yet, still, giving the Pitocin after birth seems to still help stop bleeding, even in an oversaturated uterus. So right after your baby's born, your uterus is supposed to contract down firmly. And that's what stops the blood vessels, the open blood vessels from where the placenta separated them, what makes them contract and stop bleeding. So baggy means it's not contracting properly. Okay, next question. Can you describe the hormonal process after birth and why people get the baby blues. So the hormonal process after birth, basically, to sum it up quickly, you have three major players you have estrogen and progesterone that are higher during pregnancy, particularly progesterone, right after your baby's born progesterone levels fall dramatically. And then you have a rapid increase in prolactin, which is the hormone that gets breastfeeding going and helps you make milk. So anytime we have a really rapid shift. In hormones, we have an effect on mood that can happen. So there is an underlying contributor to the mood shifts that happened in those first two weeks related to the massive change in hormones after birth. Prolactin actually is a hormone that creates a high alert state. So many women will report that on day four, when their milk comes in, they feel completely out of sorts. Sometimes they cry unexpectedly, sometimes they feel anxious unexpectedly. And that is again related to the milk coming in. And that high level of prolactin, which makes us puts us in that hyper vigilant state, which is nature's way of helping mums be highly attuned to their babies. So it's useful, but it can also be a little too much sometimes.
Yeah, and just a quick comment on what the baby blues is. It can be any combination of emotions from weakness to overwhelm, anger, anxiety, just general stress, even rage that lasts under two weeks and it doesn't affect everybody. But postpartum depression is feeling those emotions when they last longer than two weeks. And postpartum depression can happen anytime in the first year of pregnancy. And it is often linked to a risk factor like a history of anxiety or depression or a move in the family, a loss a divorce or even the loss of a pet. It that's those are often triggers. But ultimately, it seems to be linked to life change easily as much if not more than hormones, because it does affect parents who adopt 10% of birth partners, spouses get postpartum depression, you know, and just the fact that it can last can occur anytime in the first year says quite a lot. The hormones have long leveled out by then.
Yeah. And also, I think it's helpful to know that just because you have baby blues definitely doesn't mean you're going to have postpartum depression or anxiety, and to realize that it is a part of the normal physiologic transition from being pregnant to being postpartum. And your body has to go through this massive hormonal change. And anytime we have a massive hormonal change, like onset of menses, when we're teenagers or menopause, when we're later in life, or even for many people, PMS, when you have a large change in your hormones, it does impact mood.
Now, it's worth mentioning probably that we do a workshop about every month called the fourth trimester. And we get into all the details of the physical experience after giving birth. And the emotional, we spend about an hour each getting into the nitty gritty on all this. So if any listeners out there are interested in that workshop of ours, just reach out to us. And you can get on the list for the next workshop, if you just can't get enough of this postpartum conversation. Because there's there is so much to say about it. There really is yeah, there really is so much to cover. It's hard to just summarize, but it's really under discussed. That is 100%. Sure. And part of the reason that women suffer so much postpartum is that their expectations are a little bit off because of everyone leading us to believe we're going to have a certain experience and it just isn't the reality, one of the greatest values in our fourth trimester workshop, no doubt, not just what we know. But based on feedback as well is that your partner is sitting there with you, and probably the only time they will ever get an honest look at what your experience is really going to be postpartum. So anyway, there are resources like, like ours out there. And I would say definitely make sure both you and your partner are getting really educated in this before giving birth, if possible.
Alright, the next question kind of actually goes along with the first question. So let's continue. It says what kind of hormonal support is there for postpartum depression and anxiety. So first of all, we know that our first line recommendation for postpartum depression, anxiety is not hormonal support, but is human support, people connection. So, you know, some people will take medication for postpartum depression and anxiety, that's fine. Hormones are not typically prescribed for postpartum depression and anxiety. However, there are some herbs that are helpful. There are some adaptogens that are helpful, and there are some nutritional things that you can do. That's helpful and actually breastfeeding. Breastfeeding that is going well and is supported is a major contributor to less postpartum depression and anxiety. So having successful breastfeeding is one thing you can do to prevent it. We also know overall, and especially postpartum, but always in depression and anxiety, there is an inflammatory response going on in the body that impacts the brain. And there's been some awesome research done by Kathleen Kendall Tackett, who talks about the use of high dose Omega three fish oils, particularly the EPA component, official oils to decrease inflammation that has shown to be very effective at treating postpartum depression. So that's a very easy, safe intervention. St. John's Wort has also been used as well as ashwagandha. So those are two herbs and adaptogens that can be helpful. All of these things should be done with the support of a professional of some kind, whether that's a therapist or naturopath or your midwife or lactation consultant. And if you are doing any other treatments such as medication, herbs or nutritional things, you should absolutely be in a support group alongside that and that makes it more effective all around.
Okay, great. Yeah, I think that covers it Trisha. The next one says how do you get over the anxiety of having experienced stillbirth?
You know, we probably can't expect that we're going to have bringing anxiety to a zero level There's probably going to be some anxiety in subsequent pregnancies. And when it's just a matter of how we learn to work with it, how we learn to sit with it. And also just making sure that before you become pregnant again, that you really have gone through the full grieving process. We know that, you know, a mother who loses a child is never 100% over it, that will never happen. But just to make sure that you have really done the work of healing from grief, it's a process. It's a stage and it's very clear, you know how women move through it. And I think if we get pregnant too soon, that could certainly exacerbate anxiety and a subsequent pregnancy. Sometimes that might happen, you know, it might happen, but you can still work on grieving through that time. That's a hard one. But I wouldn't expect the anxiety to be completely nil.
I think the women who have experienced stillbirth who've spoken with us is community with others who have suffered. But if you do feel traumatized by any prior birth experience, there are many things you can do. And one of them is EMDR Eye Movement Desensitization and Reprocessing, which you can experience with a qualified therapist and it's a rapid way of processing trauma, but I really think a therapist anything along those lines, but again, whatever you do, make sure others who've experienced stillbirth are a part of your process.
Every expecting parent deserves access to a certified doula no matter their budget, birth plan or location. This is the idea behind the digital doula program at Beautiful Births and Beyond. Their on-demand doula program includes access to online classes and 24/7 birthing and postpartum support via text or video. Book a free consultation with founder Colleen Myatt and receive 20% off an hour of digital doula support. Visit beautifulbirthsandbeyond.com and use promo code DOWNTOBIRTH.
Recovering from a vaginal birth takes many women by surprise. Everyday activities like sitting, walking and going to the bathroom can be uncomfortable, and Postpartum Soothe is just the remedy to support your healing and relieve discomfort. That's because herbs like comfrey leaf, uva ursi and witch hazel are known for their antimicrobial and anti-inflammatory properties. Postpartum Soothe can be prepared at any time during the third trimester and it makes a beautiful baby gift. It's a must for any woman seeking a faster, easier recovery from a vaginal birth. Visit postpartumsoothe.com and use promo code DOWNTOBIRTH.
So here's an interesting one that just came up in our Postpartum Support Group this past week. And it says how can I help my husband? How can I help my hubby to learn to soothe the baby without sounding controlling? Alright, this came up in our Postpartum Support Group. So there is this interesting dynamic, because the one person, the primary caregiver of the baby, whether everyone likes it or not, has far more experience with the baby. I mean, one single week with your baby, is you've probably logged more hours with your baby than your partner is going to be able to log in the first two months. So like it or not, not everything is 5050. And I can't believe how much women struggle with this, so far as to say how many women say I want to pump only for the sake of my partner being able to feed the baby, your partner doesn't have to bond through breast milk. They have their own special ways of bonding, say go ahead. And I counseled people on that all the time in my lactation work because the they're both getting up in the night, the mothers getting up to pump to give the husband the bottle to feed the baby. And I'm like, Why are you both getting up? Why are we doing this but because I want my husband to have an opportunity to feed the baby and I'm like you're doing double the work. Just feed the baby and let your husband do something else.
It's a you're right things can be right things don't have to be 5050 in that sense at all. You're You're each going to have your own very special relationship with this child. I think we need to not worry about that so much.
And there will be plenty of time to feed the child throughout life. Right? It's not like you have to establish this in the first few months of the baby's life. Right, it easier for yourself.
Yeah. So it gets really complicated because when your partner then has an opinion, let's do this. Let's try that. You can sometimes sit there gritting your teeth thinking oh my god, I know this is not going to work. I wish they wouldn't do that the baby is going to be screaming and crying in a little while and their feelings can get hurt. Depending on who your partner is. They might go so far as to say you're controlling and it can become a really difficult point and you're in a very difficult position because you know, you know better but you know you also want them to own their parenting more. I think it's also worth mentioning no matter how convinced you are Now that you know better, you will usually be right. But there are times your partner is going to suggest something that is actually going to work out better. So I think it's a matter of them appreciating that you do have a lot more experience with the baby, but you also being able to be flexible enough to try other things. You're in this really tough spot because you don't want to look controlling. You don't want to look like you're the more important parent. And so you feel like you're gonna Okay, let let's let them have this idea. And then when it backfires, you feel so resentful, it's really hard. But they also have to appreciate you have a lot more experience with the baby. I mean, there's no right or wrong, there's no way that there's nothing to say about this, except I feel for everyone involved.
I tend to fall more to the side of I'm the mom, I'm the boss. I don't, I never felt controlling in that way. But I always felt like the authority. And then later in life, when my kids got older is a little bit different. My husband was the authority on different things, but with the infant, I don't see it as controlling to help your husband or partner understand what probably is very instinctual to you and should be because that is the way nature intended it.
Yeah, I do feel for everyone involved. Because I know if I were the partner, I know that I wouldn't want to feel marginalized. I can understand all those feelings. Yeah. And I do. I do think it's hard, it's delicate. But I the only thing I take I the only thing I have a really strong opinion about is, I don't think it's okay for your partner ever to call you controlling. And I think that that should be dealt with very swiftly. If if they start name calling or anything like that, and don't believe that you're controlling just because you're really good at what you do. That's not what controlling means.
That's that's the point that I think I was trying to drive home that this is not a time of this is not controlling behavior. You are the mom, who is going to instinctively know better, and your partner should be receptive to that.
Alright, Trisha, this one says, Do you have tips for laboring at home before going to the hospital? I'm afraid of going too soon. But I also don't want to wait too long. This is so common this question What do you say to that? Yeah, this one comes up a lot. There. I mean, there's no way to tell somebody the perfect time to go to the hospital it What? What are you afraid of, if you wait too long, having the baby in the car, that doesn't happen very often. But if it happens, it usually works out, okay. Going to soon is a much bigger problem. So going to assume getting admitted too soon before you're actually in active labor does not usually work out? Well, right labor can slow it can stall, it's not really the comfortable space you want to be in, there's more time for interventions, there's more time for monitoring, there's more time to put on the clock. So always err on the side of going later than earlier. But let's just take it from the homebirth perspective of when you call the midwife and say when somebody gets on the phone with me, and they can no longer speak through their contractions, that is the time to get to the on their way to their house. So if you're laboring at home, when you hit that point where you're like, I can't talk through my contractions anymore. I just feel like I need to get to the place where I'm having the baby. That's the time to go.
Is cord traction ever necessary to assist the delivery of the placenta? If so, when?
Well, that depends on how you talk. So we're talking to you, what do you say.
So, core traction is part of the routine management of actively managing the third stage of labor, which has been done for a long time, the active management of labor involved early clamping and cutting of the cord Pitocin administration with the delivery of the baby shoulder and cord traction to remove the placenta. This is actually how I was taught and midwifery school and you you know, you've kind of wrap up the cord and put gentle tugging pressure on it to help it separate and be born. Now active management of third stage is more modified. So we don't know. Giving Pitocin is still commonly used. But delayed cord clamping is much more accepted, thank goodness. And using cord traction, you know probably really varies from provider to provider. I'm sure there's lots of providers who still delivered the placenta via cord traction, the bursitis ends at home we don't we use gravity and upright positioning of the mom because once the placenta is separated, you really don't need to pull on the cord to get the placenta to be born. You just need the uterus to contract and have the effect of gravity. If the placenta is on its way out and you want to use the cord to just gently birth the placenta. That's okay, but it really it should never be used aggressively. You can actually pull the cord away from the placenta and create separation, which is very dangerous.
Can it also increase the likelihood of retained placenta? Yes, if you Yes, it can, because and I think that's probably separated. That's very dangerous.
Yes. So then then they have to go rescue you from the situation they caused.
Right? But because postpartum hemorrhage is one of the leading causes of death in birth for mothers, you know, it's always been, there's always been an effort made to figure out how to make the third stage, which is the birth of the placenta of safer. So active management of third stage became a very common thing to do and for a long time was thought to make it safer.
Alright, so this last one says, I just got a positive GBS test that stands for Group B strep. I had an easy fast, natural first birth and now I'm so worried should I be alright, so briefly, she is worried about a either the baby contracting Group B strep from her and getting a GBS infection post birth, or B. She is upset about getting antibiotics during her labor, potentially unnecessarily because not all GBS is even present at the time of birth. What do you have to say about it?
Yeah, so let's just review the basics on GBS, so about 1/3 of women are colonized with GBs at birth. About 50% of women who are colonized with GBs will pass it on to their newborns. And if the GBS infects the baby, which happens in about one to 2% of those 50% of those 1/3 of women who have GBS, those newborns will develop GBS, early onset disease, which can be very harmful. So we're still talking small numbers. But the recommendation is that if you test positive that you get intrapartum antibiotics to prevent your new burden from contracting early onset GBS disease. So to summarize, I would just say to this woman that you have the option of entirely declining the antibiotics, you have the option of delaying when you go to the hospital so that there isn't necessarily time to get antibiotics, especially if you had a fast birth. The first time around, as you mentioned, you didn't. And the third option would be that you opt for risk based protocol, which would mean that you only take the antibiotics if you develop a risk factor, which would be the rupture of membrane rupture of your membranes for more than 18 hours. Or you develop a fever in labor or if you go into preterm labor and have a preterm baby. So if you don't have any of those three things and you have a fast birth and your waters are intact, and you choose to decline, the antibiotics, the risk of your baby developing GBS, early onset disease is much lower. And she really has the fast birth thing going for her because most of the time when women give birth really quickly, there's no time for antibiotics. And nobody and nobody worries about it.
They don't take the baby away and check the baby. See, I've had women threatened with that.
They might threaten it, but you can say no. Depends on where you give birth. Doesn't everything. But I can tell you from I can tell you from a provider's perspective, if a woman is GBS positive, and she comes in and she gives birth within a couple hours of being in the hospital and she hasn't had time to get antibiotics and her bag of waters weren't ruptured. They're generally not worried about the GBS right, because there hasn't been a risk factor associated with it. Because we know that the risk of transmission is much greater and longer Labor's and when the bag waters ruptured longer and when you have more vaginal exams and all these things that she probably won't have time for if she has a fast birth.
Let's throw out one more Trisha, this last one says can I decline the prenatal panel at the first OB appointment. I don't want to be swabbed there are things in the prenatal panel that you don't necessarily need. But there are things that are also useful in that initial bloodwork, like your blood type, like your hemoglobin status. Most of it you can probably get away with not knowing. But getting a blood draw is also a pretty low, low risk, low intervention thing I understand not wanting to be swabbed in the vagina. Just say no to that. You can pick and choose. But your provider is going to kind of probably pinpoint you as already being a little bit.
Go ahead and say, Trisha, you know, you want to difficult, difficult and all depends on who you're who your provider is. I mean, if if somebody came to me and said, I don't want the prenatal panel, I would try to have this discussion of what is it that you're worried about in the prenatal panel, and I would probably give them the reasons that I might like to know, their hemoglobin status and their hematocrit and their blood type. And if they still say no, then Okay. All right. That's it for today. All right. Yes. So that's it for today. Thank you all for submitting your questions. We have so much fun when your questions come in, and we really look forward to answering them and remember you can find us over on On Instagram for any comments and what else?
I will see you in December. Thank you for joining us at the downtown birth show. You can reach us at down to burst show on Instagram or email us at contact at down to birth show.com. All of Cynthia's classes and Trisha is breastfeeding services are held live online serving women and couples everywhere.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social