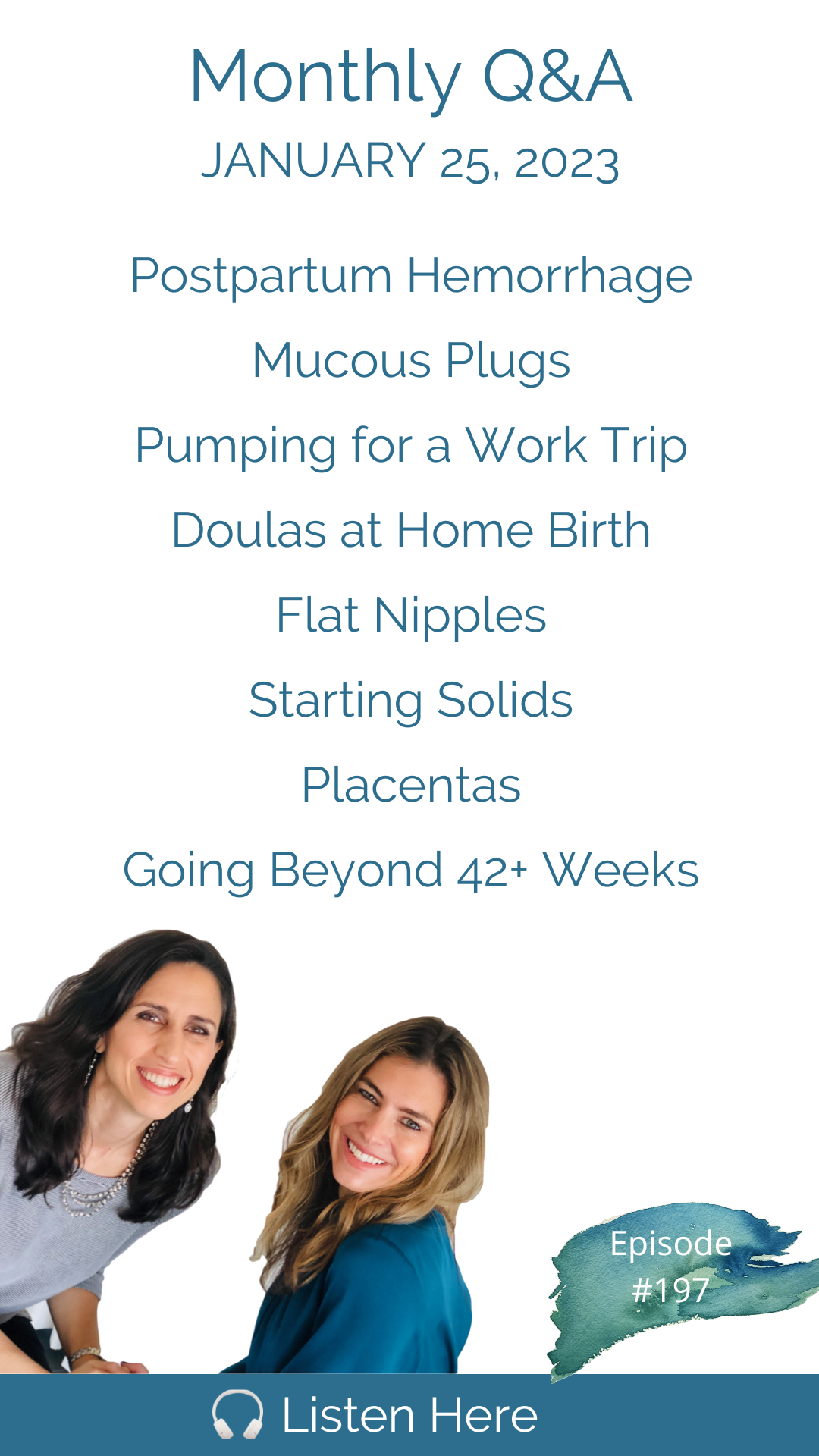
We are back with our first Q&A of 2023. We begin today by discussing absurd comments shared with us around natural birth statistics before we jump into our regular Q&As, starting with: How can I prevent another postpartum hemorrhage when I feel like I did everything right the first time but still bled too much? What role does a doula play in a home birth and how does she interact with the home birth midwife? Is it normal to lose your mucus plug at 32 weeks, and will it come back? How can I pump enough milk for my exclusively breastfed baby to leave for a 4-day work trip without risking oversupply? Is it worth it to switch from an insurance-covered nurse-midwife that I don't really like to an out-of-pocket homebirth midwife? Next, we jump into our quickies which cover topics like: oxygen at home birth, "powering through" engorgement, nipple shields, supplements for mental health while breastfeeding, flat feed in children, and - here was an off-topic surprise that came in - our favorite karaoke song to sing? And there is much more! For those who are Apple subscription or Patreon members, we answered several additional questions including: What to do in a home birth if an emergent situation arises? Is midwifery just for low-risk women? How to start solids? Is the placenta filled with toxins and is placenta encapsulation unwise? What does it mean if you can't find the heartbeat early in pregnancy? Thanks for joining us, and remember you can call our phone line with your questions 24/7 at 802-GET-DOWN. (That's 802-438-3696) Connect with us on Patreon for our exclusive content. Work with Cynthia: Work with Trisha: Please remember we don’t provide medical advice. Speak to your licensed medical provider for all your healthcare matters.
Email Contact@DownToBirthShow.com
Instagram @downtobirthshow
Call us at 802-GET-DOWN
203-952-7299
HypnoBirthingCT.com
734-649-6294
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
Trisha, we made it to season four.
That's amazing.
It is amazing considering we do a podcast every single week.
Ah, here we are. And the time has flown by I must say,
Well, yeah, we're busy. We're busy, busy women. I wanted to start by sharing a message a woman just sent us on Instagram. All right. I don't know if you've had a chance to see this yet. It is a woman from Oregon. And she says, Hi, ladies, I just need a place to vent a moment. Since I don't have anywhere else to turn. I just left my 36 week appointment where my OB has made me feel like garbage for declining interventions and certain tests, you would not accept my response of No. And when my husband later asked about what we can expect when we go to the hospital in labor, the doctor proceeded to say that any choices and choosing to have a natural labor or any choice to decline Pitocin accounts for 30% of maternal deaths. Do you hear that any choice related to having a natural labor and declining Pitocin accounts for 30% of maternal deaths? Is this a true statement? I'm feeling so devastated at the moment for his lack of respect of my decisions, and like a horrible soon to be mother for having had my own thoughts about how I want my labor to go. That's it?
Well, I guess we should start off by saying that that is definitely not true. I don't know where he is pulling that information from but to say that a natural birth accounts for 30% of maternal deaths. What I mean, what is he even talking about? Well, I
don't think he's talking about anything. I honestly think that providers like this lack the ethics to first of all, I don't I think they lacked the concern to do any research. But I think they lacked the ethics to have a real conversation with someone. And they're just truly I think he's just making up numbers. I had a mom in a hospital once after a natural birth, her partner was not even present. She had a great birth. And she brought her own oral vitamin K that she obtained from a naturopathic doctor. And the on call pediatrician came in and said, you know, 11% of babies die when they don't do the Pitocin when they don't do the vitamin K injection. And, of course it is and I ended up researching it and publishing something on it because I was I was so worked up about it. It was just an outrageous my. And it's very upsetting, but it feels real. And the thing that I wish more of these doctors understood when they do this is the part where she said now I feel like a terrible soon to be mother. What an injustice to leave her feeling like she's inadequate or an irresponsible mother only because he has his conflicts of interest and his own motives that have nothing to do with her or her intentions. And he's giving her such bad information that the only thing she can extrapolate from it is what a bad mother to be willing to risk her life and her baby's life. But we all know, as especially after our conversations with Rachel, we'd like in Episode 182. You know, she's on track all things equal for a much safer outcome if she is opting for a natural birth, especially by declining Pitocin if she has a physiologic birth, so it's a great injustice, very upsetting. So needless to say I posted a story on Instagram to see if there are any better providers in that area. And we immediately got four responses which I shared with her right away. So hopefully she can go find someone better.
Well, and also, for this mother and any mother listening, when a provider makes you feel that way, I don't care how good of a provider you think they are or what their reputation is around. But if you walk away feeling like a lesser mother, then you are in the wrong place.
So that's a red flag we haven't quite talked about. But that is true. It just means the wrong relationship. If you're not feeling good about yourself, really. We're ready to start our questions then. Right.
We are ready to start season for q&a, the first q&a of the Year. Let me just this
this month, we didn't get any from anyone who wanted to talk about relational stuff. Postpartum emotions, and sometimes those in one month.
It's rare. That's very surprising, especially after the holidays. Yeah, it's true. Oh, wow. And that, I think they think that they forget, that's an option. And all questions are legit here. So if you have any story, you want to share any interesting holiday story, even if you don't really have a, necessarily have a question related to it, share it with us, we can comment on it. Any question? Like bring that up? Because that's a really your emotional experience is a very significant part of this perinatal phase of your life. So we're here for that. All right.
Well, we were sent out I have here we go. First one.
Hi, ladies. My name is Erica. First of all, I just wanted to say thank you so much for everything that you do. As a birth doula and certified midwifery assistant, I really enjoy birth content. And so listening to your show is like a breath of fresh air. So much free information and content and education. So thank you, I did have a question. With my second child, I did have a relatively quick labor in about five hours. And even though the birth and labor itself was beautiful, it was very physiological, and I didn't have any medications. It was just very hands off, it was truly a home birth out of hospital. And the midwives there, and nurses were extremely supportive, however, postpartum, I did have some placenta membranes left behind and did have a postpartum hemorrhage, and did eventually to get a DNC. And so my question is, how could I have prevented that I truly felt like I did all of the things I could have done, I was doing a lot of things in pregnancy to help tone my uterus. And my labor wasn't one of those one or two hour ones, it was, you know, about five and a half. So not too quick. Was there anything you can suggest for my third pregnancy that I can be more vigilant about to make sure, knowing that this already happened to me that it doesn't happen again, I already planned to do the dates and the you know, pregnancy tea and the prenatal exercises, and I was getting chiropractic adjustments and massage and so many things to try to prevent this happening in the first place. And I also know things like Pitocin increase the chances of that happening, I didn't have any event and still had a postpartum hemorrhage. So if you know any other risk factors, or anything else I can do to help prevent it down the road. Or with my future pregnancy, I would love any tips. Thank you so much, again, for everything that you do. Okay. What do you say?
Well, she did say that there was a little bit of membranes left behind. So that makes me wonder if the placenta was possibly hurried or rushed in the process of birth. So even just a little bit of the amniotic sac being left behind what's called trailing membranes, if that is left inside the uterus, that can cause this kind of bleeding. We definitely know that in hospital birth, there is a lot of pressure to get the placenta out very quickly. And so if lack of patience might be the main issue here. The other thing that can happen very easily in hospital birth, it can happen in homebirth, too, but it's less likely is that as soon as the baby is born, all the focus is on the baby. And there's a lot of excitement, which is of course normal and natural. But the mom really needs to stay in her persona. Because if she sort of jumps out of that space, and loses her focus on that, then it's harder for the uterus to do its job of contracting effectively after birth. And if the uterus doesn't effectively contract after birth, and the placenta doesn't shear off the side of the uterine wall, easily, you can have retained placenta. So we want the uterus to contract effectively as effectively as possible so that the placenta can make the easiest birth possible.
We just recently talked about this on the podcast about how chord traction makes it far more likely to a want for a woman to suffer postpartum hemorrhage because of the possibility of retained placenta?
Well, that's not what, that's not actually what a active management of third stage says the cord traction is part of that whole process of the Pitocin, the cord traction, the active management of third stage, but that's really questionable research that says that the active management of third stage and low risk physiologic birth is safer, it does appear to be safer in medical births, right. And we want to just explain why because if the body isn't having a physiologic experience from beginning to end, then the body is not going to respond physiologically to expelling the placenta as easily as it will, if it is a totally physiologic experience. So if you start on Pitocin, or get Pitocin, or even an epidural during your birth, then it does make more sense to have Pitocin in the third stage of labor, but still cord traction, I mean, taking out the placenta before it's ready, that really is risky.
It depends on how much attraction you put on the cord. And if the placenta has actually separated or not, if you're pulling on it, and it hasn't separated, and you pull too vigorously, of course. But core attraction can also just mean assisting the birth of the already the are already separated placenta. But another thing to consider is the health of the mother throughout pregnancy is really important. If the blood volume doesn't expand properly, and pregnancy and you go into birth anemic, you're much more likely to hemorrhage. So it's important to make sure that you are getting enough iron throughout pregnancy best to get it through food rather than a prenatal supplement. The other thing too, is that, you know, assessment of postpartum hemorrhage is highly variable. So what's there's, you know, there's sort of this defined number that we say constitutes a postpartum hemorrhage after birth. First of all providers are really all over the board. In assessing that just like, we are assessing fundal height or cervical exams, or ultrasound for estimated fetal weight, you know, there's a lot of variation. So did she really hemorrhage? Was it just called a hemorrhage? Who knows?
What if it What if it had been.
So you have to make sure that you're well hydrated throughout labor. So if you do decline an IV, which you guys, if your regular listeners, you know, that we recommend that you have to be eating and drinking throughout labor, or if you have a really long labor, which she didn't, but in the case of a long labor, if you're not eating, if your body gets low on energy, that could also make it difficult for the uterus to contract after birth. So maybe having something to eat or drink immediately after the baby's born, that can be helpful. And just, you know, get that baby's skin to skin and taking the smell of your baby. That's a really strong trigger for oxytocin and getting the uterus to contract.
And also, we just have to say that, unfortunately, postpartum hemorrhage is not entirely avoidable this, this woman did all the right things, she did everything to stack the odds in her favor. But if she did, in fact have a hemorrhage, then we can't make that a zero possibility. In Episode 134, that was our deep dive on hemorrhage in Pitocin. On November of 2021, we talked about this postpartum hemorrhage, postpartum hemorrhage happens in between one and 6% of births. Unfortunately, I don't think we have the difference between physiologic and medicated births there. I don't know if that data is available, but the consensus is that it's at around 3%. I don't think there's any totally escaping that. But in three weeks, exactly three weeks from today, we're releasing Episode 200, which is our third fabulous episode with Barbara Harper. She's she's such an incredible wealth of knowledge. And she'll be talking all about third stage of labor like how best to birth the placenta, how exactly it happens physiologically, delayed cord clamping on the effect of separating baby from a mother and postpartum hemorrhage. So we hope you'll all be looking forward to that episode in three weeks and hopefully, we can all pick up some good tips there about reducing that postpartum hemorrhage rate even further. Which according to Barbara, we certainly can do when we when we do all the right things that are that nature and our bodies are really expecting us to do after we give birth.
Yep. All right. Hi, my name is Rio. I am a 24 year old first time mom I am 16 weeks pregnant. And we have already hired our doula for our home births that will be happening hopefully end of May early June timeframe. Have a question. So we are working with homebirth midwives, nurse midwives, and they actually require us to have a doula if we are a first time mom. I was kind of wondering what the role between the doula and midwife relationship is like, especially in a home birth scenario. I know that doulas can usually fall into more of an advocacy role in a hospital or a birth center setting, but I'm kind of wondering what our doula and midwives interactions are going to look like or if our doula really is strictly there just for us during that time. Thank you for taking the time to answer my question.
So I'm thinking that this probably comes from a very busy homebirth midwife practice, because I mean, it's not common that they require a doula for it's only for a first time mom, which to me means that they want somebody who can be there throughout early labor when the midwives may not be able to be there.
And I was wondering about that as well.
We've had this question before about is it necessary to have a doula if you're having a home birth and you have a midwife that you trust, and I am always in favor of it, I think it's a great extra set of hands. It's certainly helpful for the midwives. But truly, the doula is there to provide the mother with full time full on emotional support, whereas the midwife is going to be at times distracted with getting her gear set up, maybe she has to take another call at some point from somebody else who is in labor. If she's going to be more focused a little, I mean, hopefully, she's going to be giving the mother space in different homebirth midwives have different styles of practice. But if this midwifery practice is suggesting that you have a doula, then to me that would indicate that they want that doula there to provide that constant one on one emotional support so that they can focus more on the hands on skills of the midwife. And I would imagine that the midwife will be very welcoming of the doula and very supportive and they'll work together very well.
Hi, Trisha. And Cynthia, my name is Molly, and I'm from Madison, Wisconsin, big fan of your show, and just so grateful for what I've learned, for me to increase your wealth of knowledge. I'm a first time mom with a 10 month old but I'm actually calling on behalf of a friend who is currently 32 weeks pregnant, who is also a huge fan of the show. So anyway, a part of my friends mucus plug came out at 32 weeks, which initially was pretty concerning. And we'll we did some reading. And we saw that sometimes mucus plugs can come out early and then regenerate. So it's not always a cause for concern, but to talk to your provider regardless. So she went to one of her scheduled OB visits. And she talked to her OB and VOB said that she wasn't concerned, but that also some people say that the mucus part isn't even real. So we're wondering what your thoughts are on this. We, I've always heard that losing your mucus plug can be an early sign of labor as it was, for me, I think I lost my couple of days, or maybe even a day before my son came, you know, and some women lose it during labor, etc. But neither of us have ever heard that it just straight up doesn't exist. So again, we'd love to hear your thoughts. And we are just huge fans of the show and so grateful for everything you guys have taught us and empowered us to do.
It's real.
The mucus plug is real, as a real thing.
We're not 100% sure that it came out, right. That was what the mother assumed. But if it if it did come out, I think it would indicate she might because it often can come out in little pieces and no one ever notices it. But it's possible that if something came out that it was only part of it in the first place. It's possible she was a tiny bit dilated, but it could Yeah, weeks before Labor begins and a woman can dilate a bit before Labor begins as well for weeks several centimeters sometimes, but can't just reform anyway, if she doesn't go into labor.
Yes. So the mucus plug has just a bunch of gunk that fills up. Lovely. I mean, I could go into all the details
during seal and the HypnoBirthing by the way, the uterine seal, we don't like plug I mean the language is just horrible. Whoever came up with all this language. It's not a plug at all it's lug it's like the size you are now we need the seal is a much better way to describe the uterine seal that no one knows what you're talking about. But it feels a lot better to think and to say. Alright, so well. Here's the thing your cervix is like imagine like a squished doughnut, like the hole in the doughnut is squished together and that little teensy tiny bit of openness in the squish center of the donut has to be filled With something to protect anything from ascending into the uterus.
we have a new name.
All right, well, now you're at least always going to imagine your cervix looking like a squished up glazed doughnut. And that little space is filled with this stuff that forms the mucus plug in as your cervix starts to open, that is released. And yes, most commonly that happens as an early indicator of labor. So at 32 weeks, that's early, and you know, I think she did the right thing by checking, checking in with your provider making sure there weren't any additional signs of labor. But in the absence of contractions that are progressive and getting stronger, she's fine.
Hi Trisha in Cynthia, my name is Amber and I'm from Bend Oregon. And my question is in regards to adding something into my well established breastfeeding routine. I am planning a work trip and I will be gone for about four days my daughter at the time of the trip will be about seven months old. So this isn't in a month's time. She is exclusively exclusively breastfed she does not take the bottle she has tried receiving a bottle from my husband and then also from my mother in law who is our nanny. Unfortunately, she will not take it I have about 20 ounces storage so far. My question is how do I introduce pumping into my daily routine without disrupting one her feeding schedule? She feeds about six to eight times today. And then also how do I ensure that I do not create a situation where I have an oversupply because this late in the breastfeeding game. I don't want that to happen. The detail that I need to know is how can I add 100 about approximately 160 ounces to my stash so that she has an adequate supply while I am away I think I will be gone for days but it could be five thank you for all that you do and I really appreciate you answering my question like a four day work trip. That's a long stretch of time to be with your baby and to provide enough milk for four days in advance of leaving means that you've got to get your body producing this extra which she said she needed. 180 ounces. My recommendation general Ellie is not to store more than about two, maybe three ounces of milk per day so that you don't get into an oversupply. So she would need almost three months of storing milk to store up that much milk. Then when she goes away in our trip, she's gonna pump another 180 ounces of milk while she's away and come home and store that milk and have nothing to do with it. So, you know, not that there's nothing you can do, you can use that milk, you can donate it, you can do baby baths with it, you can make food with it there, there are things you can do. But my point is women get themselves into stressful situations where they feel that they have to, and sometimes they really do have to have all this extra milk stored up. And then oftentimes, it doesn't even get used. So it's complicated. Leaving a breastfeeding baby. I guess that's what I'm in a very roundabout, long winded way to your answer is two to three ounces a day is all you recommend. And if that's impossible for her, because she hasn't been doing that, you're saying she's at risk of oversupply. So what should she know in that case, if she does have to save more, so if you drive up your supply higher than that, which would take adding additional pump sessions, after the baby feeds to increase your supply, so to store a couple of ounces per day, you would probably only have to pump after one or two breastfeeds each day and store the extra milk. If she had to drive her production up by eight extra ounces a day to catch up and save up enough milk by this time. That would require a lot of pumping.
Anything to be aware of to avoid over supplier there is no avoiding it. You need the extra milk you need your body to go into that mode, right?
Yes. But if you get into oversupply, there's a lot of complications that can come from that. So you don't really want to go down that path. So I say you store two to three ounces a day. And you store what you can. And the next best thing is that you overnight your milk wire away. That's the better thing.
That that's a great idea that I never thought that it's worth it. It's a nuisance. It's expensive. No doubt. It's nice. But yeah, that is an option. Good. Great. Because the stress of thinking like that's that's usually what I recommend when it comes down to more than about 24 hours away. Okay.
Hi down to birth girls. This is Kathy. I'm calling to leave my q&a. So my question is related to due date, and the rules or laws around them. I am currently pregnant 33 weeks, and I live in Florida. So I know every state can have different regulations. From what I understand. If I go past 42 weeks, then I can legally no longer birth at my birthing center with my midwife. And I have to birth at a hospital, which I'm assuming I will be pushed into being induced, I find this so frustrating that because of you they can use like a best gas. And I don't want to be in a hospital setting where interventions are going to be pushed. So what's the twist now? An at home favor, because no midwife can legally attend the home birth because I'm past 42 weeks. I just feel so conflicted on what's best. And what to do. Because in my heart, that's just how I feel. Just feels like the system does not support women. Appreciate your time. And hope this question helps other women understand and make decisions that support them. Thank you. Yeah, we faced the same situation. And I personally faced it policy. And when I was birthing in a birth center the first time around, yeah, it's a lot of stress, to have to worry about that. It is what comes with birthing in a birth center. And most places you need to focus on plan B does that mean you're going to have a home birth as Plan B or that you're going to prepare for a hospital birth, the odds are not high that you'll go best 42 weeks, but you they like think they're fair, there's a fair chance of it, you very well may go past 42. So you just have to get more comfortable with your plan b It's a shame to impose these hard lines. It's a lot of pressure.
Well, in some states, it's illegal for homebirth midwives to do home birth after 42 weeks. So it's limited very limited in some areas. And this is part of what's driving some of the free birth movement. Now we have known women to work with their midwives to alter their due dates slightly. Right? We know like birth center midwives are a lot less likely to do that. Okay. We have to sort of usually report to the hospital or keep the hospital totally apprised of what's going on. So it's not a little wink wink that you have between yourself and a home birth midwife in most cases where there's no such oversight.
Yes, but also, women need to make sure that their original duty that they were given is actually accurate based on their menstrual cycle, because just going by the standard Nagle's rule doesn't apply to everybody's cycle, some women have longer cycles, some women have shorter cycles, and you have to take that into consideration, because that can alter your due date by however many days short or long year cycles, so you need to go convince them that you have a 33 days back, oh, wait a minute, I forgot my cycles, actually 37 days, every month, that month, that was I remember, that's how that works. Yeah, that one month, that one cycle, it pushes it out by that number of days. That's interesting. So in your case, in your example, it'd be an extra nine days added to the like, estimated due date, your cycle length is a is a factor. And it I mean, if you just have one random long cycle, that's probably not the case. But if there's a high probability that the cycle was long, then your ovulation date would be later, there's a good chance you'll have the baby before that, it's the stress of thinking about it, that's really the problem. And you can also empower yourself by planning all the ways to induce labor naturally, if your baby is close, then you'll get that baby, you'll get things going before 42 weeks, I did once have a mom, a client who went to 43 weeks and four days, and from 41 and a half weeks on, she was doing all the right things to get that baby out. But the baby was nowhere near ready, maybe because of her cycle. But I think you just have to get comfortable with Plan B, whatever that is, so that you can reduce any anxiety and stress and circular thinking around this because that is where the problem comes is when you're just not feeling good anymore, and you're anxious about your birth, which is what we do not want, you're better off just letting go of it. And trusting yourself to manage your hospital birth. If it does come to that and just letting go of this concern. It's unless you have other options like going to another state for your birth, which some women do. Alright, next.
Hello, my name is Rio and I had a question for you guys kind of regarding some thoughts I'm having about switching midwives. I am currently under the care of a nurse midwife practice here in Colorado Springs, Colorado. And I I did not have a very good experience with one of their mid nurse midwives in the rotation that they have, it is very likely that she will attend my birth as to the other midwives are pregnant right now as well. And I just really would not like that energy in my home in my birth space. And I am definitely thinking about exploring other options. And I've gotten lots of good recommendations for other midwives. The only catch is, other midwives do not take insurance. And that is a big reason why I am thinking about using the nurse midwife practice here in my city. Can you kind of give me the pros and cons in your mind about what would be the benefit of switching midwives versus a cost of using the nurse midwife practice versus a licensed midwife? Thank you.
I think the only thing i The only thing I would say to that is that it really just comes down to personal cost benefit to you of having the birth experience that you are most desiring versus risking your birth being altered. I mean, if you're not prepared for it, and it's not financially feasible, it's just not feasible. But is it worth spending the money on? We would I think both say yes, I mean, we talk about how you should plan your birth, like you plan your wedding, like, well, she only said that she doesn't totally love her current practice, but she didn't necessarily say she loves the next group that she found. So if you do love the next group that you found, and it feels right to you, and if you do have the money to spend on that, and we don't know if you do, if you do, then it does seem to us that your intuition should guide you as long as it isn't cost prohibitive. I don't think just running from the current providers to any other group or going into debt is something we would say go ahead and do I don't think that would be the right thing for you. you first have to assess whether you absolutely feel right about the other group. Before getting into the decision about finances, you just first have to ask yourself if that's the right group. So we don't know.
I would say it's worth even borrowing money from a family member. If, if they're willing, if this is so much what you desire, and you feel so off with the group that you're in, I think that would be worth it. But you have to, that's why it's so personal, you have to weigh the cost benefit to you and the stress of the financial piece of it. Nobody can make that choice for you.
I talked about this in my HypnoBirthing class yesterday, because I ended up leaving my doctor and my first pregnancy and I switched to the birthing center and there was a young midwife there who was very cold. And I never felt good in her presence. She never made eye contact. She never smiled. She always seemed to be in a bad mood. I absolutely prayed I wouldn't get her I loved the other midwives, and I got her. And it's a little bit of it was a great life lesson for me now that I'm teaching, but the doctor I fired had a far more charming disposition than the midwife I ended up birthing with. But the lesson I learned was that the midwife I ended up birthing with ADD, she served me perfectly. She wasn't warm. I wished she had been. But she only spoke twice during the birth. She said the perfect words both times and I realized after my son was born, she wanted the outcome I wanted, which wasn't the case with the other doctor. So when we hear a woman saying, I'm not sure I like this midwife. i You definitely shouldn't birth with someone where you don't feel safe. But keep your wits about you. As far as do they have the same birth intention? Are they being negative about my birth plan? Are they saying things to pressure me intimidate me misinformed me? Or is it just like you just don't love their personality, but you absolutely respect how they practice so that it's just so complicated. And that's why I think the whole thing starts with you what your intuition is telling you about who whose hands you belong in for your birth. It's, it's it's something that another person truly can't answer for you. So I don't know if she hasn't met these other midwives yet, but I if she hasn't, I think she asked to start there and listen to her gut.
Look how much you had to say about that. I guess I did. All right. Good.
All right. So for those who are not with us on Patreon or Apple subscriptions, in which case we have, I believe 767 Additional questions in the extended version this month. It is time for quickies then it's quickie time. Okay, here we go with January quickies? Does induction with Pitocin actually make labor more painful?
Yes, notoriously, yes.
Yes, it does. Next, should I use a nipple shield or nipple shells for inverted nipples? Well, quickie. Yeah, that's a that's not a quickie the answer to that. But they can definitely impede your baby from learning how to latch more deeply. There are some very specific circumstances where they can be helpful, but I would not jump on a nipple shield for inverted nipples. The Lansinoh latch Assist is also a great device for inverted or flat nipples. That helps if I hurt them, it's like little suction cup that pulls them out. Okay, next. Okay. Help. My husband just doesn't understand anything I'm going through.
We know. That's all I have to say. Yeah, I was I was out to lunch with my mom today. And we were talking about this. And she said, I don't think even the most loving, supportive husbands can possibly understand. And I said they could they simply can't just as I didn't understand, before I had children, my sister in law did and I, I didn't have the insight into what her lifestyle was like, I couldn't possibly I would hang out with them and just think she was the same old person as always, but it's a How can anyone understand so you're, you can talk to him about it. But you also have to find women who understand it where you feel like you have a little bit of a more understanding audience.
You can also leave the baby with him for a couple days. And that will scratch this that will scratch the surface on what your lifestyle is like because even even if you which most women don't do, right, it's just a little sampling because even if you do that, no one understands the fatigue and waves of potential downhearted misled, say when when it's 24/7 like that reprieve is not coming. So anyone can get through a couple of days but to feel like am I ever gonna get a break? How many years is going to be that is a particularly hard role and that is usually the role of the mother very difficult. So we understand. I don't think we've Have any advice? We just we absolutely understand. And there wasn't a question anyway was there? Call in and give us more detail on your situation, we'll answer it in the q&a with a more lengthy, detailed response.
Next, or we can do an episode with both you and your husband. And we'll just kind of talk it out and see what you have to say and see what he has to get out. Maybe get a nice conversation going. I'm sure that would be helpful.
Do I need to wear a belly binder after an external cephalic version? No, no, you know, best supplement for mental health that is safe for breastfeeding. Fish oil. Fish oil has been shown in high doses of the EPA component of fish oil to be as effective as antidepressants for postpartum mothers. Wow, that's very interesting. Anything else like vitamin D or something?
Well done. That was a just right quickie. Was should a midwife always carry oxygen to a birth? Yes. In my opinion, yes. If the baby needs oxygen, the baby needs oxygen. You want to have that? Does your milk supply dip when you are sick? It certainly can. It often does. Depends on how sick you are. Some people read through it pretty easily. The more sick you are, the more impact it has on your milk, your body's got to decide in that moment, what it's going to fight what it's going to put its energy toward. So if you're super sick, your milk supply may take a bigger hit, but it's usually temporary. Especially if you have a healthy milk supply. You can come back as soon as you get better. You must also stay hydrated. That's one reason it can also dip is that when we're sick, we tend not to drink as much liquid. Can you ovulate postpartum with no period? You can, but just once, because once you ovulate, you'll get your period. But you can be late before you get your first period. So the answer I would have said based on what you just said is no but keep in mind that you will ovulate two weeks before you get your period you won't ovulate for a month and another month. You if you're not if you don't have your period and you suspect you've been ovulating. I don't know what she means if she thinks she's just been ovulating all this time for a few months without getting a period. Right that you would say no to that, right? Yes. Okay. Yes, it's in order. That might have been her question, right.
How do you push through engorgement while breastfeeding? That's a quickie. I guess the answer to that is that encouragement that happens on the third or fourth day is a normal physiologic process that you don't need to push through. You just keep on breastfeeding. And you can use some cold compresses to for comfort, encouragement that occurs after anytime after that time is more pathological. And you should call an ibclc because there's a underlying cause that needs to be addressed. Last quickie. What is your go to karaoke song?
It's usually something by Alan's Morissette.
Which really reward Yang. Oh, it's the it's incredibly hard to sing. And it's so much fun because her songs are so passionate and fun. And what's yours? country song? But don't you love Madonna? I know where you and I have such big differences. Hey, like a virgin. I was never a Madonna fan. I never realized her the opposite for me.
I should yeah, I shouldn't say idolized. But she was when she talked about one person that I would listen to over and over and over again.
Yeah, it's really weird ending to the episode. And it wasn't quick. No, now we're just talking. You guys are like guys wrap it up. Okay, so we want to make sure everyone knows that we've got a lot going on over on our Patreon platform. This is our community of our most enthusiastic fans and followers. We meet with you twice a month on a live stream webinar. You guys can join on screen. So when you have questions you jump on but we just did one on postpartum rage newborn interventions. When you get into that into that page, you see every live stream we've ever done in your feed, but then you're with us twice a month when we keep doing new ones and access to extended episodes and everything like that. So that is to us about things like our favorite music, you can message us directly and we will get right back to you personally. So um Yeah, I mean, we're booked out on birth story sessions for a couple of months, but we're also doing man birth story processing sessions. But check it out, go to patreon.com/down to birth show and just see what's over there we have downloadables which are really cool and episode index all our extended episodes, just a whole lot more time hanging out with us seeing us behind the scenes making all our mistakes and no editing possible. It's good, it's growth for us Trisha, it is growth for me to have no editing capabilities on that platform.
And there will be more coming on Patreon over time so it's a place to evolve and grow with us.
So with that said, Have a lovely end of January and a lovely beginning of February. And we will see you we will catch you next week.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social