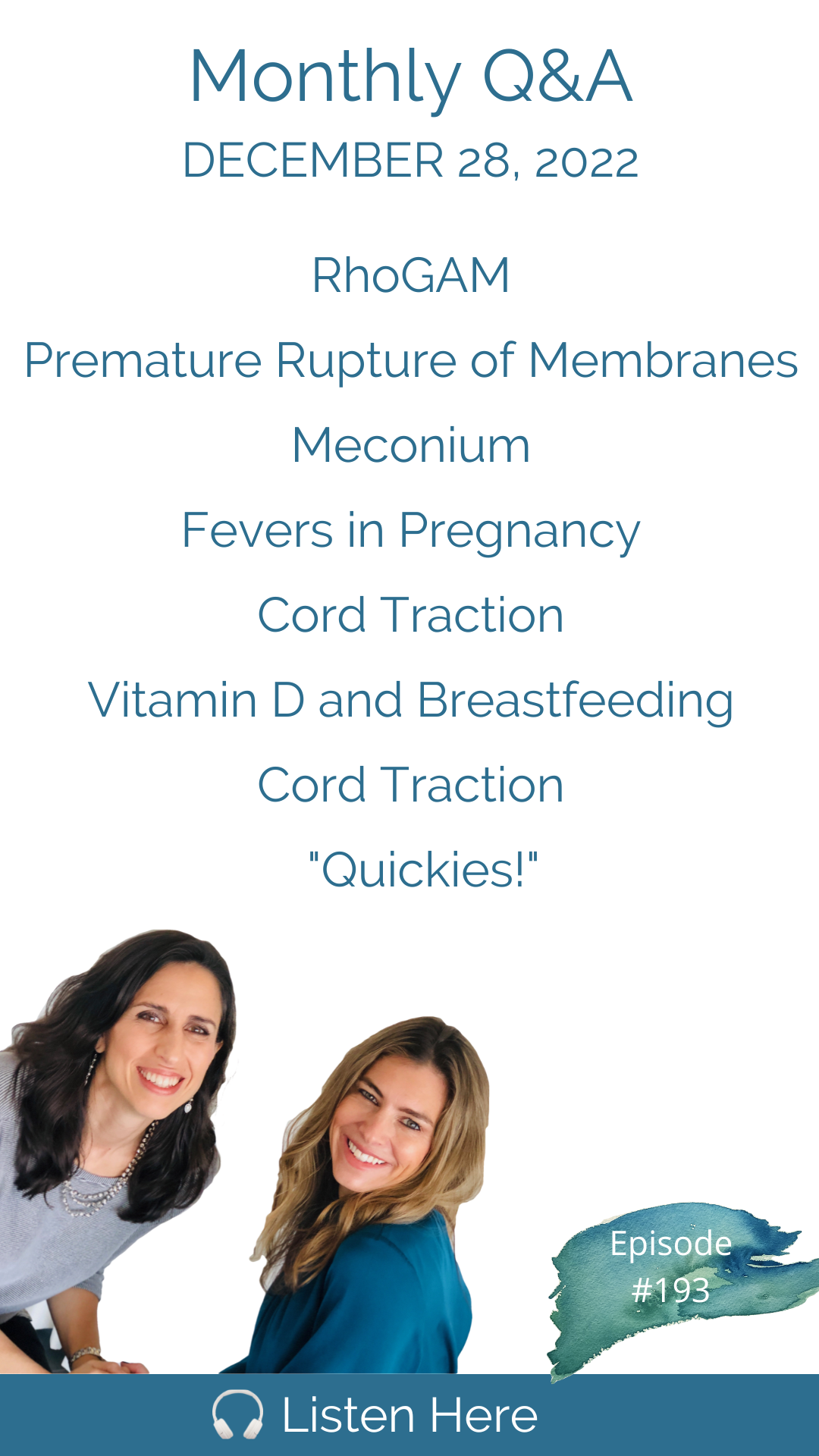
Hello everyone! It is that time of the month, and we are back with our December Q&A. To kick it off, we have a follow-up conversation based on one listener's response to episode #188 on Rhogam. Next, we jump into our questions discussing the actual risks of going past 24 hours or ruptured membranes without contractions and how you can mitigate those risks. We break down why meconium becomes more concerning after 42 weeks gestation and what those actual risks are. One mother who has the flu in the third trimester wonders if this is harmful to her baby and what she should do about it; another mom is curious if it is more helpful or hurtful to use assistance to birth her placenta and questions if a hep-lock or IV port is really necessary in labor. Furthermore, is vitamin D supplementation truly necessary for breastfed babies? Additionally, we have a great quickies segment on pregnancy headaches, aging placentas, newborn rashes, breast changes in pregnancy, cold-plunging postpartum, water birth and infections and whether or not sleep training babies is really needed. In our extended version, over on Patreon and Apple Subscriptions, we dive into a very important topic: How to accurately calculate your due date based on your specific menstrual cycle, not the average cycle. We discuss delayed cord clamping and where to clamp the cord, two-vessel cords and the implications for induction and the safety of home-birth with midwives who have restricted access to emergency medications. It's an extra-long extended episode this month - happy new year! Remember you can hang with us twice a month during our interactive and educational livestream for our Patreon community members! Connect with us on Patreon for our exclusive content. Work with Cynthia: Work with Trisha: Please remember we don’t provide medical advice. Speak to your licensed medical provider for all your healthcare matters.
Email Contact@DownToBirthShow.com
Instagram @downtobirthshow
Call us at 802-GET-DOWN
203-952-7299
HypnoBirthingCT.com
734-649-6294
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
We've been working on it for three and a half. Right? Yeah, we're going real are three full years of episodes going into our fourth season. Very exciting. Anyway, I want to read this email from a listener named Kelsey. I thought this was really worth worth sharing. And I really appreciated that she wrote this. So she wrote. Hi, I Cynthia and Trisha, I'm reaching out about your recent episode with the mama who was RH negative and her story. I'm also an Rh negative mom with an Rh Positive husband. My children both are Rh positive. I received Rogaine with my first during pregnancy and after birth. With my second I questioned it a bit more and did a lot of research and in the end, I decided not to receive programs during my pregnancy, or after my birth. I will be getting bloodwork soon to see if I was sensitized during my second pregnancy. One big concerning factor for me with the program, especially this time around was the fact that it is a blood product from multiple people, meaning one dose is composed of plasma from more than one person. I dug and dug and could not find any information that factually stated If program as plasma from donors who have received the COVID shot. The reason I'm reaching out is first to thank you for shining light on this topic as it is very, very under researched and families have to really dig to find the information. My midwife and I had to really work together to gather the facts. I'm also reaching out as I would love to see a follow up episode focusing more on the risk benefit analysis of Roe Gam itself. This is a product that is administered across the board to any woman who is Rh negative. There is such little information so of course there are even less informed consent conversations happening. I had an ER visit during my pregnancy because of some light spotting. And the first thing the doctor said not asked was alright, so you will be getting Rogaine. He did not even ask my husband's blood type. If my husband's blood type was RH negative and I just said okay, I would have received the shot for no reason at all. A really great resource on this topic is Dr. Sara Wickham. She talks a lot about it and wrote the book anti D explained. As an Rh pregnant mama, it was definitely a very tough decision that caused a lot of stress and worry because of the little and sometimes conflicting information out there. If I were pregnant now and in the decision making process and listen to your episode, I may have decided to take the program out of fear. Of course you need to hear both sides in order to make an informed decision which is why I'd love to hear a discussion where that outcome was different from the one in the episode. Thank you so much for what you do. I'll see fair points worth talking about testing this doctor, they are sometimes routinely recommending rogram. For women who are RH negative, it totally regardless of whether the husband has Rh Positive a non issue if if he writes negative, that shouldn't happen. But the reason that people don't talk so much about the risks of getting rogram is because the risks of a baby getting sensitized in a future pregnancy are so severe. And because the incidence is so high, I asked her that and she said, there's conflicting information on that, too. You know what, it's very possible that there isn't good information on that, because everybody gets rogram. So there's so few cases of people who don't get it that how would we really be able to know that nobody's studying it except who? She said, Sara Wickham has written a book on it. And Sarah, if you're happen to be listening to this episode, we are trying to get you on the podcast. I haven't heard back. She's very hard to read. She has started to read I heard you we we want to talk about vitamin Trisha wood and Rogaine with you. So, especially because this mom, Kelsey read Sarah's book and came to a different conclusion.
Yes, I think I think that's the thing that did, nobody studies it, and nobody talks about it, because everybody gets it. Because that risk is much higher than a lot of other things that we make choices about in pregnancy. And so it just becomes a non issue for most people. And I mean, interestingly, though, in the episode that we did the program didn't work at all. That's true. Nonetheless, mothers should be informed that it is a blood product, and what the ingredients are in it, and what the risks of getting the vaccine or vaccine, it's like a vaccine, getting what the risks of RhoGAM are. And it goes beyond just risk of infection and pain and bruising at the site of injection.
Yeah. All right. You're rare. They're rare, but you still have a right to know, of course.
Alright, let's get started. Great.
Hi, guys. I have just a quick question. So I know a lot of times when your water breaks, or when you think your labor, they kind of put you on that clock, that seems like the magical number, from what I've heard is kind of 24 hours, and then they want to push other options. Just why do they do that? I guess, is there any rhyme or reason to it? Or is it just more out of convenience? Or? I don't know, I guess it's my first my water broke. And I called them and they told me immediately I had to come in. And they said, if I didn't have it within that 24 hour mark, they were going to start intervention. So I guess just curious why they do this.
Thank you. Well, we've touched on this a few times before, but it's always worth mentioning again. The 24 hour rule basically comes from the fact that 90% of women who break their water before contractions begin will spontaneously go into labor within 24 hours. So that's sort of become the cut off that if you go beyond 24 hours, you're outside of that 90% And you're not normal. And so every buddy wants you in labor by 24 hours. The risk of infection also goes up at 24 hours. So that's, that's the standard of care that you induce or augment or get labor going at 24. At the 24 hour mark to prevent the risk of infection when infection if it's not GBS, all the infections that women can get from all those unnecessary cervical exams, you mean?
Yes, exactly. Yes, you can live. Without it, you can still develop a choreo or an infection in the uterus without having GBS for sure. Right. But it is reduced significantly if you keep everything out of the vagina. So once that bag of water is broken, now, anything, any bacteria that's in your vagina, on your skin on somebody's hands on any device that goes inside your vagina is potentially introducing that into your body into the amniotic fluid, and now there's potential risk of infection.
And we It's also worth mentioning that this there is there's no evidence to support speeding up labor or getting that baby out within at the 24 hour mark. And you Trisha is talking about that statistic related to once membranes release, but what women are facing is arriving at the hospital and that's when the clock begins and we have a local hospital right here in Fairfield County, Connecticut, that quote gives women 10 hours, and at 10 hours, they start pushing C section and they want to see as my doctor said to me, I want to see you dilate a centimeter an hour. Well the heck with that. There's no research supporting any of that. So this is all rhetoric. Everything we're talking about is rhetoric except the part Trisha said about infection. That's, that's definitely worth knowing. But there's no good explanation. And we can't, we can we can theorize, but we can't support or explain why these policies are there. They're not serving women and their families that we do know.
As long as your baby's doing fine, and you are not developing a fever, there's just no good reason to aggressively push labor. Just wait, keep waiting, it'll come, it will happen. I mean, if you're not in that first 90%, you're pretty likely in the next 12 to 24 hours to go into labor.
Hi, Trisha. And Cynthia. My name is Regan, I am 37 weeks pregnant. And Ashley from Manitoba, Canada. I have a question for you regarding the conium. So my question about my podium came up quite early on when it came to appointments with my midwife, because I was born at 42 and four, seven pounds and six ounces. Obviously, I wasn't a big baby to be born over 42 weeks. So I was talking to my midwife about it. And she didn't bring up all the usual things that I've heard, like, the big baby thing or the fluid, they were the pelvis, she brought up that the baby would start inhaling the conium. The longer it goes over 42 weeks. The other thing is, is after 42 weeks, I don't have the option of bursting out of the hospital anymore. So the Freebirds or in a hospital, and she would not be happy at all if I went over 42 weeks. Yeah, I just wanted to ask you guys if going over 42 weeks in the conium is as big a deal as she was making it down to be? Or yeah, if there's not if it's not as big a deal. Thank you.
So the risk with meconium later in pregnancy, after 42 weeks is that the baby one is more likely to pass meconium and two that your fluid is likely to be less. And that combination increases the risk of meconium aspiration syndrome, which is very severe. It doesn't mean it's going to happen. But you put those two things together and the risk goes up. So that's the concern and babies born at 42 weeks and beyond have a higher incidence of meconium aspiration.
So in your opinion, does we normally when women are being pressured into induction at 42 weeks, it's a lot of talk around stillbirth. Are you saying you think it's reasonable justification to to routinely induce a woman at 42 weeks just because of the concern of meconium?
No, I'm just saying that the risk goes up. But no, I'm not saying routine induction at all. I don't know the percentage right off the top of my head of meconium aspiration syndrome at 42 weeks, but I think we'd be hearing a lot more pressure about that if it was greater than the risk of stillbirth, which is, you know, mostly what we hear. But if you have usually when you go that late in pregnancy, you are doing some sort of surveillance of the baby like a biophysical profile. And if on a biophysical profile, it was determined that you had very low fluid, then maybe you would consider those risks differently.
According to medical news, it says that meconium aspiration syndrome is a rare complication that, according to the International Journal of Pediatrics affects .18% of full term newborns. Okay, that's a very small number that's like less than a fifth of 1%. That's a very small number. That's 18 per 10,000.
So we're talking about a risk that's still half of what the stillbirth risk is at 42 weeks. So yes, the risk goes up. But again, we have to always look at what the actual numbers are. And not just the relative risk.
I mean, this if you if you just flip it for a second, we're talking 99 point 99 point 22% 99. Over 99.2% of women are not going to experience this and we're talking about a woman who's who has a family history of having babies later. So 18 Pretend 1000 is 1.8 per 1000. So we're talking about one per 500 babies.
Hi, ladies. I have been battling the flu for the last couple of weeks. And I am just curious. Thankfully, in that time, I've only had a fever, a low grade fever once and then again today, but I'm just curious how it's hard to find information on fevers and third trimester and how concerned I should be and what I should be doing. If anything I tend to just let my body do what it does, naturally. And I don't usually take anything to lower my fevers. But I also want to make sure baby is safe.
My perspective on this is you're not seeing much about this, because it really isn't as big a deal. That's as its lead, as we're all led to believe. There's a lot of rhetoric around this, but your body heats up to kill the virus, it's not affecting your baby, you get the flu, it feels miserable, it feels crummy, your baby is just fine in there, we're led to be afraid of getting the flu, some people say the flu is worse than getting the vaccine. But in fact, there's a lot of controversy around the vaccine. When you get the flu, you've got to take care of yourself, I believe in letting the fever do the work as long as you're able to sleep and rest. And if you're staying very well hydrated, and hopefully taking really good supplements. But the baby is sitting there collecting antibodies, which is a beautiful thing. And when the baby's born, your baby's going to have all those antibodies. So that's what's happening for your baby, while you're while you're laid up in bed suffering, your baby is strengthening,
I would only just add the one thing is that if you develop a really high fever that can cause increased heart rate, or tech or cardio, and it might be worth taking a fever reducer at that point. I mean, I'm all for letting the body burn it up and write it out. But in pregnancy, sometimes we want to just have a little lower threshold. And you can take time you can take Tylenol, what would be the threshold in your mind like one to two and a half? 103?
Yeah, probably. But you know, it depends on how long it's prolonged to have such a short interval of time that it's high, then fine. But if you're really enduring a high fever for a long period of time, it a little dose of fever reducer is probably better than not.
Hey, ladies, my name is Shelby and I am six months pregnant with my first but I guess I kind of have two questions and feel free to only answer one. And that's a lot. But my first question is around the delivery center. And kind of this idea of assisting it by my OB, she mentioned it was routine. And I know routine is not necessarily good word. And she's been really open to all of the other things that I've proposed, that I wanted to do. And so the question is, is like, is there really any benefit to the light assistance? The delivering of the placenta? Are there downsides? And then my other question is around the I guess it's called a hemlock or they inside the IV. She seems like a really want to use one of those did not pushing IV but I feel like it's one step from IV I'm really concerned that that means that other types of interventions might be pushed. With that kind of being a gateway intervention. I really appreciate your thoughts on those. Thanks.
Yeah, this is really important stuff.
They're both great questions. So I think we have to answer both of them. Absolutely. So as far as the delivery of the placenta, it's sort of funny, because back when I was in school, which is now 18 years ago, 18 Yeah, 18 active management of third stage of labor or active management of the placenta was the that was what we were being taught that's clamping the cord, giving the Pitocin cord traction to birth, the placenta. Now, it's sort of like, okay, well, everybody knows that delayed cord clamping, clamping is better. So we'll let that part of active management go, but we still have to do something. It's like they can't quite let go of just letting the placenta be physiologically born. So what she's asking is, is a little bit of traction or a little bit of active management of the placenta unnecessary.
It's not, no, it's just not. And what concerns me is, I've been talking about this more and more in my HypnoBirthing classes. There is a real trend right now, in routine manual extraction of the placenta. And I find this to be absolutely appalling like that, to insert the whole hand slash arm lower arm into a woman to pull out the placenta. I can't believe this is happening at the rate it's happening. And I've done some research on this and it absolutely is causing more harm than good. There is a much higher risk of infection, a much higher rate of postpartum hemorrhage, possible genital tract trauma. So when we're having these if you're very flexible with a doctor who quote likes to do this stuff, I'd be careful. I would really err on the side of saying I don't want assistance birthing my placenta, my body is going to expel The placenta Now obviously, if something comes up, you would change your mind, as is your right. And you could get assistance. But I think you're in a better position to draw kind of a hard line around that so they don't start messing with you. It's not supported by evidence. Cochrane did it. We did. Cochrane had research on this. Did I say that right? That word, Cochran? Cochran did research on this? At some other Yeah, because it also increases postpartum endometriosis. It's really problematic. It's really problematic.
So when people are looking for ways to try to reduce postpartum hemorrhage, postpartum hemorrhage is the leading cause of maternal death worldwide, right? It's the it's the riskiest part of birth. So it's really hard for providers to not feel like they have to do something to ensure that that placenta is born as swiftly and safely as possible, when really, the right thing to do is not intervene during the labor and oversaturate all the oxytocin receptors, so that the body can do its job postpartum, and effectively contract and stop the bleeding. So we try all these different things to see if we can do better at birthing the placenta faster, because the longer the placenta sits there, the feeling is that the risk of postpartum hemorrhage is higher every minute we wait. So there's this sense of urgency to get it done.
The research is currently saying that there's a higher risk if the placenta doesn't count come out with an hour, and a new aren't normally comes out quite quickly. But I just want everyone to understand the common sense behind it so that it makes a little bit of sense to you. If you're listening. When a placenta comes out naturally on its own, it's attached, think about it in tag attached to the inside of your body through open capillaries, this is how blood is getting transmitted, right? It's blood. This is how everything is getting transmitted from the mother to the baby. It comes out on its own only because those capillaries pinch and seal off, which is how that placenta detaches itself. It doesn't rip itself out with these open capillaries where all the bleeding is happening. That is what happens when they reach in there. Nevermind What a miserable experience that is for any human being. When they reach in there and take it out all those capillaries are exposed and open. And that's why that procedure is linked to higher rates of postpartum hemorrhage.
Because your body has to produce a massive amount of oxytocin when that placenta detaches in order to contract the uterus down effectively enough to seal off all of those capillaries. So this is a major reason why it's so critically important that after your baby is born, you do not lose your focus, your birth is not over, you have to stay in your birth zone. So that your body can stay in that safe, quiet, calm space that we were just in. While we give birth to the baby, we have to remain there through the birth of a placenta. And so often after the baby is born, it's kind of like we're snap out of it, the lights go on the people come in the babies taken away. How do you expect your body to stay in that zone when all that excitement and actions happening around you. So then the placenta takes longer to be born because you're not staying in that safe nest to allow the oxytocin to do its job.
And a quick word about how blocks, they are not linked to safer birth outcomes. I do believe it's the first step and unnecessary interventions, they can get women in an emergency situation if they had to. Even when women need emergency C sections, it's so often a part of their story that they're sitting around waiting for the surgeon to show up or they're sitting around waiting for the paperwork to sign. And there's a lot of pressure on this, but headlocks nevermind IVs we're just talking hep locks which is attached to nothing, it's just a catheter in your vein. These aren't linked to safer outcomes at all, you do not need one. If you want to give birth with a catheter in your vein, go for it. But this is not linked to better outcomes. It's just, in my opinion, a really unnecessary way to tether you. And you're going to be much more likely to receive intervention if you have it. It's your personal decision, but there is no evidence to support this. I Trisha I have to tell you someone in my class the other day, said that she was told she would need to have a headlock and she was pushing back a little bit. And the provider said to her if we don't give you a headlock and labor your veins will collapse. Because we're not going to feed you or hydrate you so called Have you ever heard that? Well, that's what happens when you get dehydrated. So collapsed. But what does collapse mean?
What do they keep they means they they go they go you know how when you are looking for a vein you want it to be protruding and bulging so you can get a cat an IV in there and when you're dehydrated they get really flat and they're hard to access. So that's what they're saying. But that's silly.
Well, he read her me terrified her. She thought, oh my gosh, this sounds like something I have to do, right? Like, my veins are gonna collapse and I'm not going to be able to breathe anymore. It's going to cause something horrible to happen within my body. That's just not true. Right. Next.
Hey there. I've been listening to your guys's podcast for the past several weeks of my pregnancy, several months actually, and has been so good. I do have a question. I've heard some women avoid dairy or other foods while breastfeeding. This includes alcohol, due to the way their baby reacts. Can you explain why someone would avoid certain possible allergens and or how you would know how to avoid them? Thanks, guys.
Basically, the way I see it, and I'm sure I'm gonna learn a lot in our upcoming episode in our upcoming interview. But my, my training and understanding about allergens and breast milk is that whatever the mother is highly sensitive to food wise, so she has an allergy to dairy, wheat, corn, soy, whatever it is that she's more likely to produce antigens when she consumes those foods and the antigen itself that her body produces can sometimes leak through into the milk ducts and be transferred to the baby. It's more likely to happen in moms who have abundant milk supply or oversupply or lots of engorgement, it's like the the ducks get a little bit more leaky under pressure. So it's very common with oversupply to see babies have allergy type reactions and breastfeeding, which can be colic. Reflux, rashes, eczema, excessive fuzziness, that kind of thing. The most common culprits are dairy, soy, corn, wheat. So it's really common for moms who have any complaints about their babies for their pediatrician to say, you should cut dairy out of your diet that's like the go to get rid of dairy and dairy is the number one culprit. But I like to take a step back. And you know, there could be some underlying breastfeeding issue that the pediatrician is not picking up and picking up on it's not always a food allergy, it might be a hyper lactation issue. And if you're not sensitive, particularly to dairy, you've never noticed you have an issue at all with it.
Hi, Cynthia and Trisha long story short I had a beautiful VBAC. And it was only detected two weeks ago that I actually had a cervical laceration. I had a slight postpartum hemorrhage that was quickly controlled with the use of Pitocin. And my provider is a an osteopathic doctor, and she said that she would have to look into the implications and whether to repair or not. I currently don't know if we want another child. That is up for debate. But I'm wondering like, what are the implications? What are the risks of having a cervical laceration? I know it has been linked to incompetent cervix, which I know we don't love that term. But I you know, there's some information out there about whether you should have a Susteren before you go into labor. So it's just curious what your thoughts are, of course, I'm going to see what my provider says. But in the meantime, I would love to know your thoughts.
Okay. So the risk here with having a cervical laceration is in a subsequent pregnancy, there is would be the consideration of the you know, preterm labor, preterm birth because the cervix would not be staying closed and tight. However, this does not pan out in the evidence. There was a study done back in 2016, which showed that there was no difference in preterm birth rates for women who have cervical lacerations in a prior pregnancy, and that the management of care of her pregnancy should not be altered in any way. So she doesn't necessarily she certainly doesn't need a C section. She doesn't necessarily need progesterone or sir collage, which are the two things that would be most likely offered to prevent to keep the cervix closed and prevent it from early dilation.
Yep, and I reached out to Tara Gibson, and she said sometimes that pelvic floor, physical therapists can help with lacerations. So it just depends on the laceration on the laceration. But they, but they absolutely do work on these.
The cervix heals, just like any other part of the body, just like the uterus, it heals. And there's no such thing as an incompetent cervix. That's just terrible language.
Hi, ladies, I'm wondering if you have any thoughts on the use of the Doppler, particularly to check the heartbeat in the first trimester around 10 to 12 weeks, I'd prefer to use a fetus scope, but I know it won't pick up the heartbeat that early. And in the first 10 months, I just want to hear the heartbeat and have some confirmation that everything's going okay. But I'm concerned about radiation and want to limit that. So just wondering if you can share your thoughts. And any thing about the safety of using a doctor thinks, Oh, if only every provider knew how to use a fetus scope.
I know what is the big deal? This this aversion to it, it's such a lovely means of getting the heart rate.
And you hear the heart rate actually in a natural way. It sounds like a real heartbeat and not this amplified sound that comes through the Doppler. However, yes, it is harder to get it earlier on, we can certainly get confirmation of heartbeat much earlier on with a Doppler or even earlier with ultrasound. But yeah, there's some risk of exposure. What that is exactly. You know, nobody's talking about it as being a real major problem, but it's not benign.
Yeah, more and more research is coming out on that. Now. The point is, I mean, Doppler is less than ultrasound. intrauterine ultrasound is the most these higher tech ultrasounds now have more the duration that you're exposing the baby has more. And we're not saying this to distress anyone because virtually everyone is getting ultrasounds. But there is good reason to not get any ultrasounds unless you really need to or want to, I mean, the anatomy scan makes sense for a lot of people. But after that, just to keep checking on the baby with ultrasound, you really can turn those down. And if you don't, there's research to show if you're getting unnecessary third trimester ultrasounds, that is linked to dramatically different birth outcomes. And we'll cover that in one of our upcoming live streams on Patreon Trisha because there's really good meta analysis to show the bad information that comes from that. So Doppler is you know, you can view it as a it is less exposure than an ultrasound, you can view it as a necessary evil, you can choose to get it and not let it bother you at all because the risks are still debatable. Or you just decline you can decline those as well.
Right? You don't have you definitely don't have to have that. I think your point about duration is really important. Many people are just going to want confirmation of the heartbeat. It only takes a second you hear it beat a couple times and you can turn that thing off. You don't need to sit and listen to it for a minute. And that's a Doppler Doppler. Yeah, yeah. Or even with ultrasound. Yeah, the moment they see it, you can be like that's it. I'm done, and the provider is happy because they get to bill for that one.
Right. 10 seconds.
Everybody's happy. All right, next.
I had a question about vitamin D supplements for breastfed ease. I feel like I'm getting conflicting information where my breast milk is everything my baby needs, but I also need to be supplementing with vitamin D. So I was just wondering your thoughts about it. All right, thank you.
So yes, your breast milk should have everything your baby needs. But the issue is that human adults are not always as nutritionally replete as we should be. Many of us are deficient because we eat highly processed foods and our soil is deficient in many vitamins and minerals. And we certainly don't get enough outdoor exposure. So most of us have low vitamin D. Therefore, we can't expect expect the breast milk to be sufficient in vitamin D. So the recommendation is that babies receive 400 I use daily vitamin D via dropper if they're exclusively breastfed, formula fed babies are supplemented in formula with vitamin D. Or if a mother takes, I believe it's 5000 5000. I use daily vitamin D, then her body should have enough vitamin D to sufficiently provide vitamin D for the baby via the breast milk.
Alright, let's get to quickies.
Okay, how can I combat early pregnancy headaches?
Other than sleep and water?
Eat more frequently. Don't let your blood sugar get well, that's the main trigger of headaches in early pregnancy is low blood sugar. And that happens really easily. So eat at least every two to three hours, smaller meals more often. How do I talk to my OB about aging placentas not being a thing, you don't need to talk to your OB about this, their mind is already made up. If they were interested in this, they'd be listening to our podcast episodes with Rachael read or they'd be doing the research on their own. So the question isn't how to convince them. They have to convince you of things. You just have to do your your research, make up your mind, and then manage your doctor. That's all you have to do. Create your boundaries and manage your doctor. You're not there to convince anyone of anything. It's actually the reverse. Next.
That's all perfect. All right. Is 26 weeks too late to switch from a birth center to a home birth midwife? Oh, of course not at all. Oh, that's early switch. Go.
I've had couples switch from one provider to the next after 40 weeks. Wow. coming to mind right now. In fact, one of them message me today on Instagram.
So no, you got plenty of time. Is that a red flag to spend eight plus hours in a birth center after a car crash and only see the midwife one time? Wow, that sounds concerning. So she was involved in a car crash. Went to the midwife's office to have the baby checked. I'm sure I'm just assuming this is the story. And we did. Was there for eight hours to be monitored. only seen by the midwife one time, I would say yeah, that's concerning, because that just indicates that they are over. Booked understaffed. I mean, that's a long time to leave you.
I mean, maybe she was hooked up to some kind of monitor. And there really wasn't much to be done, though. And maybe it's not the nicest, but maybe it's not negligent carry there, because there was probably like a nurse watching the monitor or something.
Yeah, you still think you should be seen by your midwife more than once in eight hours a hug or a stroke of the head something please.
Yeah. I mean, it's a it's a precautionary sign.
I mean, the only question is, how did it feel really?
Right? And has Have you felt that way? Again, since it's kind of like a fluke. It's kind of like, if you give birth with like, a doctor or midwife, and you feel like, you love them so much. And you feel like they cared about you so much. And they see you six weeks later, and they're like, you had a boy, right? You're like, what? You haven't? You haven't been thinking of me and my baby every day. Yeah, that's these little moments can really sting.
Okay. Our little bumps on anyone's face normal? Very likely. Yes. I mean, newborn skin is so full of little bumps and color discolorations. And rashes are so common in newborns, their skin is very sensitive. So absolutely. And by three weeks of age, don't forget that newborn acne is a real thing. Yeah, usually clears by five weeks. And I always say don't schedule your newborn photos between three and five weeks, because it happens to all of them. How do your boobs change as you get closer to delivery? They don't actually change that much.
I can get a little polish throughout pregnancy, they can get a little by the end.
Yeah, a little bit. I mean, they sort of changed throughout pregnancy, your nipples get darker, your breasts get fuller, things become more sensitive. But there isn't like this massive change right before delivery. Right there is on the fourth day when your milk comes in. That is massive. That is a massive change. Can waterbirth increase the risk of urinary tract infections? No, ma'am. And when people will tell you that it can, or people will tell you that it increases the risk of infection overall, and it does not sit on by that. If you don't sleep train, will the baby eventually sleep the right number of hours? Yes. Without a doubt.
Yeah, by college, they'll be sleeping all the time.
Just wait till they're teenagers. They're exhausted. Okay, plenty of sleep.
Yeah, I mean, sleep training, though. There's an aversion to the word training. And I don't love it either. But like, if developing good sleep habits with the baby can serve you and your baby really? Well. It's not just a function of how many hours they get. But how much restful sleep you're all getting. Anyway. Yeah, it's a hard question to answer. Honestly, I don't know what to say to that.
I don't think you have to sleep train. If you're having major sleep difficulties and something feels really abnormal, then you could look into some sleep support. Yes. But you don't have to train them in order to get them to sleep the right number of hours. What are your thoughts on cold plunging for detoxing six weeks postpartum? I am breastfeeding as well. That's bold.
It's great for the immune system. It's great. But how on earth is that practical? Are you gonna do a cold plunge?
Maybe she has a club called punch?
Maybe she does. What do you think of that in front of her house? Um, I think that if it feels right to her and her body feels ready for that it's similar to like returning to exercise when you feel ready. Goes start. Slowly. Don't sit try to sit in a cold pool for five minutes. Maybe you do 10 seconds. You build up to 30 seconds you build up to a minute as long as it feels okay to your body. It's fine. It's not gonna hurt anything. Would you do it?
And I wouldn't do it under any circumstance. Now. I would like to. I try to I try to make the water in the shower cold sometimes.
I've started doing that. I finished every shower with a cold cold no I started cold I can't finish cold.
Oh no. You have to do around it starting a cold is miserable. But we know finishing durable. No, because you're hot then and then the cold actually feels okay.
But then you finish the shower and you're shivering whereas the other way you end up nice and toasty warm.
I get so cold so easily. You know that about me? Yeah, but when I do a cold finish to my shower. I'm never cold when I get up. Not at all. I feel so invigorated.
Oh, wow. It's super healthy. Try it that way. Switching water doesn't get that cold. It's like my best brownie is that's really part of the problem. It doesn't come to my house. Oh my gosh, I'm your house. This comes from hundreds of feet down. But it's so cold. Ours doesn't get that cold. Actually, it's not hundreds of feet down the ground. It's not that cold but because it sits in the pipes on the surface. It is really cool now are we done? That's it. All right. So you know what we need to say? My bedtime we need to say Happy New Year. Oh my gosh we need to say happy healthy, successful, joyful, spectacular, fulfilling beautiful New Year and 2023 make all your dreams come true in 2023 and bring on Season Four.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Hey there to my two favorite East Coast birth ladies. It's Lee calling you from kawaii Hawaii, where this evening and most evenings I am incredibly grateful for the fact that our night skies here are so clear. There is no ambient light and the stars are always so special blessing to you and much much thanks for all you do. Aloha
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social