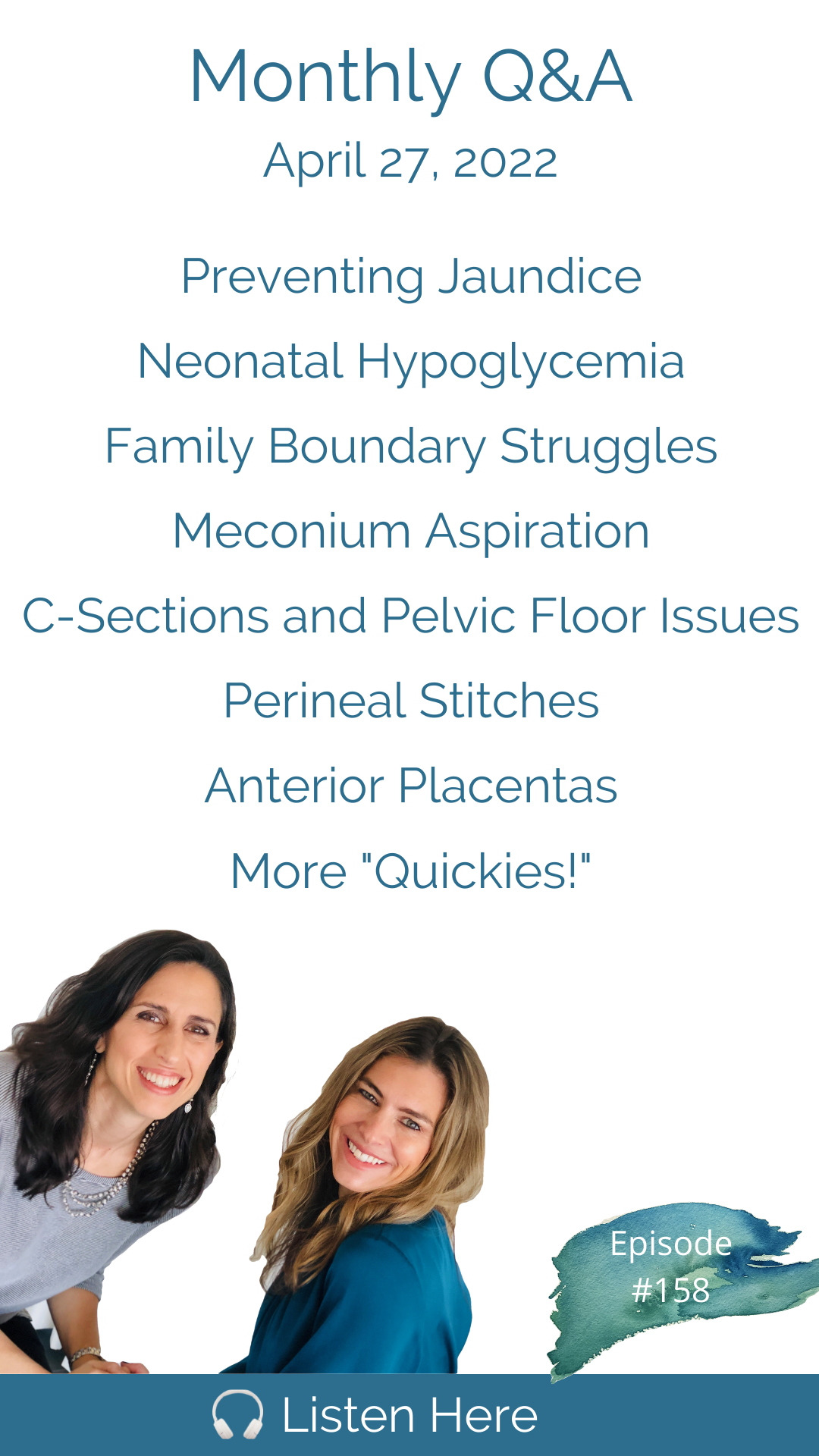
It is time for our monthly Q&A episode! This month we kick it off with a follow-up conversation on the impact of early, frequent breastfeeding on significant jaundice. Next, we address the question of why babies who are born "big" get heel sticks for blood sugar monitoring; the impact of a c-section birth on your pelvic floor; how to manage family boundaries around your birth and birth preferences with your sister and mother-in-law; if you tear during vaginal birth and get medication for stitches, is it still considered an unmedicated or natural birth? Is there a way to monitor your baby's heart rate and still be able to move freely and change position? Will an anterior placenta impact my labor? Tune in to catch all these great questions and more. Thank you to everyone who submitted questions for our monthly Q&A. If you have a questions for a future episode, please submit on our website downtobirthshow.com * * * * * * * * * * This show is sponsored by: Connect with Cynthia and Trisha at: Work with Cynthia: Work with Trisha at: Remember - we're in CT but you can be anywhere. We serve women and couples coast to coast with our live, online monthly HypnoBirthing classes, support groups and prenatal/postpartum workshops. We are so grateful for your reviews and shares - we love what we do and thank you all for your support! Please remember we don’t provide medical advice, and to speak with your licensed medical provider related to all your healthcare matters. Thanks so much for joining in the conversation, and see you next week! Support the show (https://www.paypal.com/paypalme/cynthiaovergard)
Connect with us on Instagram @DownToBirthShow, where we post new information daily related to pregnancy, childbirth and postpartum. You can reach us at Contact@DownToBirthShow.com. We are always happy to hear from our listeners and appreciate questions for our monthly Q&A episodes. To submit a question, visit the Down To Birth website or send us a voice memo through Instagram messenger.
Silverette USA*
DYPER*
NOM Maternity*
Serenity Kids*
Wildbird.co*
Beautiful Births and Beyond*
Postpartum Soothe*
*Use promo code DOWNTOBIRTH
First of all, if you tear you don't necessarily have to be stitched many first degree and secondary degree tears do not need stitches, you all have to remember nature has you covered. Nature does not need all the stars to perfectly align for a wonderful safe birth nature is prepared for all the variations that can happen. This tale is told to route our community and scares many people, including my husband away from having a baby anywhere other than the hospital. What causes meconium aspiration? Is it preventable. When you have a C section, you're cutting through the abdominal muscles which are connected to your pelvic floor, you can have just as many pelvic floor problems as you would with a vaginal birth, sometimes worse.
But that was a pretty powerful moment. For a woman who was about to become a mother the rest of her life, you know, you need to have those moments where you say, Wait a second, I'm not. I'm not telling you this so that I can see if you agree with me. I'm telling you this as a courtesy.
I'm Cynthia Overgard, owner of HypnoBirthing of Connecticut, childbirth advocate and postpartum support specialist. And I'm Trisha Ludwig, certified nurse midwife and international board certified lactation consultant. And this is the Down To Birth Podcast. Childbirth is something we're made to do. But how do we have our safest and most satisfying experience in today's medical culture? Let's dispel the myths and get down to birth.
We are back and we have a lot of questions here swimming in questions. It's exciting. It's wonderful. Thank you all for submitting so many great questions. We are very excited to answer these tonight.
And we're staying true to our new segment that quickies segment at the end, where we answer as many questions as possible at the end of the episode just firing off our answers. But these are the deep dive questions. Trisha. I don't know if there's one or two q&a episodes ago that we were talking about what you had posted on Instagram, with respect to the immense benefits jaundice wise, avoiding preventing jaundice. And in a mom breastfeeding as basically as many times as possible. Did you say in the first 24 hours? Can you explain that again?
Yeah, well, there are. It's not just John as benefits. There's just a tremendous amount of benefit to breastfeeding more often in the first three days than most people think is the norm, or the advice that they get to just, you know, breastfeed a few times in the first few days. But there's a, there's a direct correlation in how many times you breastfeed in the first three days and the level of significant jaundice that your baby might have at day five or day seven.
I feel like this is an important topic because when you hear about jaundice, I know that the typical recommendation and hospitals that my clients have heard is get your baby on formula. I don't really understand jaundice nearly as well as you do. But they say get your baby on formula, and it will make them basically poop and help get rid of the bilirubin in their intestines.
Is that right? Yes. But it doesn't have to be formula. It just needs to be food.
Well, I know. And it sounds interesting to say like it makes them poop more because that might mean that I don't know. It's like whatever it's doing to their system. That's how they're trying to get rid of it. But colostrum actually is known research, like in research to actually be the best remedy. Just keep giving your babies colostrum.
Colostrum is by far and away the optimal and perfect food for your baby in the first few days. The reason that formula will be suggested is because you can control the volume, and it's about volume. So if your baby doesn't get enough volume in the first few days, the jaundice is likely to be worse. So if we can push formula, we can ensure volume. With colostrum, we don't know, we don't know exactly how much how much your baby is getting in. If they're not going to the breast 10 1214 times in 24 hours, they may not get enough, therefore, that's why they say good formula to get rid of the jaundice blend. In fact, you really just need to get them at the breast more.
Well, this mom wrote into us to confirm and validate what you already know to be true. And she wrote Hello, I'm listening to this week's episode and I just wanted to comment about the jaundice piece that I had where I had the exact experience that you both talked about. No one told me prior to my first birth how much the baby needed to breastfeed in the first 24 hours and my oldest ended up having to go under the lamps to be treated for jaundice. For my second and third. I nursed them constantly for those first two days and while they both had mild jaundice, neither needed to be treated. Actually my third was a preemie. The nurses kept telling me to feed him every three hours, but I fed him about every 30 minutes, the midwife on staff came to check on me and confirm play instincts to keep nursing as often as possible. You assuring me, he would be fine. And he was he spent no time in the NICU. And we were released early from the hospital. My biggest tip for breastfeeding friends is do as you said, feed them as often as possible in the first 24 hours.
So depending on how your birth goes, it can be tricky sometimes to get your baby to feed frequently enough, in the first 24 hours. If you had a medication and birth, the baby might be extra groggy if you had a really long labor, or they might be extra groggy. If you had a difficult birth, a C section birth, they may have a harder time being stimulated and woken up to feed that frequently. But this needs to be the intention, it can't be that we say oh, don't worry about it just the first 24 hours, they're fine. You know, they can go a long time without food. Because then they're going to end up on somebody suggesting that they go on formula. So if the intention is to breastfeed, we need to understand that it is normal for a baby to go to the breast 1012, even 14 times a day in a 24 hour period. And that it benefits them not just that day, but in the coming days. It benefits your milk production, and it reduces jaundice.
If we had a holistic health care system, obstetricians and nurses would have to have breastfeeding education. But we don't. And because we don't, it would just be much more helpful if everyone acknowledged the fact that they don't. And to say, well, let's see what a breastfeeding expert would say about this. But the problem is we're all crossing these boundaries. You have doctors giving nutrition advice, they don't study nutrition, you have nurses giving breastfeeding advice. They don't study breastfeeding, you can't have the wrong person giving medical advice. So that's really the toughest thing, because when you're sitting there in the hospital with your baby, everyone looks like an expert next to you. So well. All right. It was good to hear the personal account, right?
Absolutely. We always love to hear that. Thank you for whoever written and share that with us. Her name is Megan. Thank you, Megan. Alright, so shall we get into our first question? Yep. All right, here it is. Hello, ladies. First, I can't thank you both enough for your podcasts. I've listened to almost every episode at this point. And it has helped me totally transformed my approach to my pregnancy, labor and birth. My question has to do with big babies. And she put it in quotations. So she's we know she's a listener. My first was born at 41 and a half weeks at nine pounds, 13 ounces. And I'm currently pregnant again. I loved having a big baby and I'm crossing my fingers for another big girl. After I birth my first daughter, the hospital staff tested her blood sugar several times in the first 24 hours. She wasn't showing any signs of distress, and I was never diagnosed with gestational diabetes. I didn't know any better at the time, so I just agreed. But I hated seeing them prick my brand new baby. I assumed it had something to do with their size. But why did they do this? And if I have another big baby, is this something I should consent to? Well, we can say that it's routinely done when you have a big baby and you know how we feel about routine. Cynthia, tell them how we feel about routine routine is a red flag word. All y'all didn't we say it was the most dangerous word in obstetrics? Yes, it's the most dangerous word in obstetrics, nothing should be done without cause without a reason for doing so. So to routinely check these things, is usually where the risk outweighs the benefit, as this Mother's intuition is leading her to already suspect. So here's why it's routine. Because when you have a big baby, there's an assumption that there is an underlying or misdiagnosed gestational diabetes, and that the baby is going to suffer from low blood sugar because the baby has been growing in an environment where, you know, blood sugar has been too high for too long in pregnancy. So you can have a nine pound 13 ounce baby and not have gestational diabetes.
One in 12 babies is quote, big with the definition of big being greater than 813. But that's really interesting. They just make that assumption. But okay, that's the assumption. So she didn't say she didn't say anything about having gestational diabetes, she wasn't. They just assumed that that's what happens. And so they start testing blood sugar. And, you know, instead, they could just make sure that your baby is nursing often enough, there are concerns of with a baby having too low blood sugar, it is a very, it is a very dangerous situation if a baby has too low blood sugar. But if the mother does not have gestational diabetes, and the baby is going to the breast and does skin to skin after birth and is getting physiologically regulated with the mother after birth, there is no reason to assume that the baby is going to have low blood sugar if the baby's not eating that's different story.
Right That makes sense and just to satisfy any curiosity out there. There are two key and primary reasons babies are quote big And that is genetics. And it's how nutrient dense is the food that you eat, because it benefits the baby to pack on weight and the weight of your baby gestational diabetes aside, the weight of your baby is not correlated to the ease or difficulty or outcome of your birth. If big babies went in your family like they run in my family, that's you're likely to have a big baby. And the only other thing that moves, that needle is nutrition, you can have a thriving baby that's very, very small, because that's simply your genetics.
It also has to do with length of gestation, she was 41 and a half weeks, she was almost 42 weeks. And we know that babies can put on half a pound a week in late pregnancy. So I feel like something to do with it.
I think it can have something to do with it. But I also think they're on just a different trajectory. It's like every 14 year old is a very different height and weight and my daughter was nine and a half pounds born at 39 weeks to the day and it's kind of like my body said this baby is ready. Like it's you can go into labor now. So yes, but most babies that 42 weeks, way less than my baby did it 39 weeks. Yes, absolutely on totally different trajectories anyway, but that baby, of course, is getting half a pound a week. Right? Whatever, you know, whatever scale they're on. Alright, let's hop over to the next question. All right. Cool. All right. The next one says Do you have tips on healing slash strengthening the muscle, the muscles after a C section. I'm 10 weeks postpartum, and my pelvic muscles are still sore. I have aching and pain. No one tells you about pelvic floor recovery after this major surgery?
This is a great question because most women think that if they don't have vaginal birth, they're going to have no vaginal issues post birth. Right. So sometimes women will even elect to have a C section because they don't want to have any damage done to their pelvic floor. And what we know is that regardless of whether you give birth, vaginally or abdominally, your pelvic floor is impacted. And we just did a great episode with Sarah, the pelvic floor specialist, also known as the vagina whisperer, whose episode will be coming out on May 11. So right, okay, great. That's a great episode.
Yeah, it's gonna be a great episode. And we talk a lot about this. But we've we have talked about it before on the podcast that just because you don't give birth through the vagina doesn't mean that you're not going to have pelvic floor dysfunction. And because when you have a C section, you're cutting through the abdominal muscles, which are connected to your pelvic floor, you can have just as many pelvic floor problems as you would with a vaginal birth, sometimes worse. And I want this mom to also know that 10 weeks is nothing very early Monday, you have time to heal to make a full recovery. And in fact, many pelvic floor specialists say don't even come in to start working on this for a few months.
I believe they usually recommend that if you're still feeling discomfort at three months, so she's about two weeks away from that, that that's the time when you want to when you want to come in. But yes, it is still. It is still I wouldn't necessarily say normal, but it is still common to have aching and pain at 10 weeks. And a pelvic floor specialist, pelvic floor physical therapist is the next best step so you can learn exactly how to gently recover the pelvic floor. Strength and structure.
Okay, the next couple of questions are about one of everyone's favorite topics, family boundaries. I never know how helpful we are. But we keep getting these questions. So I guess we must be saying something that's satisfying sometimes on this topic. But we got so many and we're going to be two of them. The first one says Hi there. I'm pregnant with my first and my mother in law said, oh, I want to be there for the birth can I be? I don't have to be in the room. But I want to be there. She lives in another state. So I presume she would intend to stay with us leading up to the birth. I don't want her here. She's a narcissist. Wow. She's a narcissist and makes everything about herself. Even when we told her some names we picked out she said, Oh, I don't like that name. That doesn't go with your last name. Or I can't pronounce that name. Why would you name my grandbaby? Something I can't pronounce. What can she not pronounce? I don't know how to tell her she can't stay with us and that we want to be by ourselves for the first two weeks. You know, the thing with out of town family is when you do see them. They're overnight. They're 24/7. And when you have family nearby, people think sometimes that's the bigger struggle but when they're nearby, they're really short, sweet visits typically and no one is moving in with a suitcase and staying with you. So you know what no excuses Airbnb are everywhere. You can easily book an Airbnb and it doesn't have to be that way. I know that that might that's obviously not what the mother in law wants.
No, but I was thinking of like women in my postpartum group who say things like, Oh, you're so lucky you're so and so's live far away. And it's like, well, not necessarily because of course they see them and when they do, they're moving in for a while.
Like my mother comes for two months at a time. Oh, come on. Let's Be honest, this year was like three months. It was three months this year. I was lucky. She is your mind's like mid March and she's still there for Christmas. Really? Just one more week. All right. Family boundaries. Alright, here's the next one. On the same topic. Do you want to read this one? I don't.
Yeah, sure. Let's go. I'll read it. All right. How do you handle family and get them to understand a different mindset when it comes to childbirth? Question mark, exclamation point, question, mark, exclamation point. I'm 19 weeks. I just told my sister and one of the first things she said was, Can I can I be the sister? Yes. It'd be fun. Okay, just told my sister and one of the first thing she said was, are they going to let you go two weeks over with this baby?
I snapped and said they don't get to let me do anything. Since it's my body, my birth and my decision. As long as, as my baby and I are healthy. I fired my old OB. And that's why I'm seeing a new OB and hiring a doula. She didn't say anything more. She also said some harmful and hurtful things prior, not meaning to you. She just runs off at the mouth. And she could tell I was already upset with her. This isn't the first time she's made comments like this. And it's so frustrating. I've made it clear that with my first baby, the hospital screwed up my husband, I trusted them and we shouldn't have I had an emergency C section due to failure to progress. My sister almost defends them when she wasn't even there. I'm just so annoyed and I need to vent. All right, so we have a mother in law and a sister. Let's start with the mother in law.
I think we should introduce these two to each other.
I'm sure they get along swimmingly. Well, let them share all their opinions with each other and not with the family members who they're stressing out. You just you know, we never know when we have new listeners. And we never know how informed our listeners are. We know after we know most of our listeners, they seem to be very informed when we hear from them and when they reach out to us. But it is worth mentioning right off the bat failure to progress is basically a doctor's opinion that the labor has gone on too long. And it is the number one reason for cesarean section in the United States. It is not a medical indication, that is the issue we take with it. The doctor that I ended up firing in my first pregnancy said I need to see you dilate a centimeter an hour and she expected full dilation within 10 hours that is absolutely ridiculous, not remotely supported by evidence well and was supported by the Freedman curve of long ago, which has long been refuted as so yes,
long ban but she also but in the same conversation, she acknowledged to me that she didn't care if I labored at home for 20 hours before getting to the hospital. So I think right there, she lost credibility on that point. Even at the time I was selling in formed, I knew things weren't adding up. But you know, Trisha pointed out in the recent episode, that something that was I thought so important that many women are told they've achieved failure to progress, when they're not even in active labor yet, like they're calling failure to progress at five centimeters, you can eat, you shouldn't even be evaluating anything at that point. But in and of itself, that is not a reason to perform this major surgery. So I think the biggest problem that this mom got, or this woman got herself into is having the conversation with her sister in the first place, because it kind of invites the discussion and the opinions. But clearly, she's had to process a C section, she didn't feel it was necessary, and that's painful. And if you can't talk to your sister about it, for God's sake, right, it's like a trap, you want to talk to your family, you want to be able to tell them how you feel. And then it's opening this door to opinions in some relationships, which isn't appropriate. And and it is It isn't right.
And obviously, she and her sister come from different perspectives about birth one has more inherent trust in physiologic birth and the other seems to not, and isn't wanting to support her sister in her and her birth goals. So this is where you have to decide to set those boundaries and and just say that, you know, this isn't something then that you're going to continue the conversation with her. If she's not going to be supportive of this. Then this is an area where you and your sister might just have to take a little bit more space during this time.
Yeah, it's okay to tell her that you're not interested in having the conversation with her. No complaining no explaining why you the really the real trap is when you start explaining your decisions to other people. That's where you're opening it up. Patricia, what's the phrase you love? There's a phrase I love to but what's the phrase you love?
Their opinion is none of my business.
And the one I like is I actually it just came out of my mouth once when I had to say it in a situation once about my own decisions, not to my own family to my in laws, who are very loving and caring people who initially didn't understand our choice to switch to a birthing center. And it was getting a little intense and I thought they would be all happy and supportive as my family was and they weren't and not initially they weren't And I remember saying, Look, we don't have to come to consensus here. We didn't tell you so that we can all come to agreement. And if that was the end of it, they were very supportive after that moment, but I felt really bristled because it was a big deal to us that we made that change. I never knew anyone who birth with midwives before it felt really radical to me, and I needed a lot of support. But that was a pretty powerful moment, for a woman who was about to become a mother the rest of her life, you know, you need to have those moments where you say, Wait a second, I'm not, I'm not telling you this so that I can see if you agree with me. I'm telling you this as a courtesy, basically, right.
And that's the whole thing. If you believe in what you're doing, you truly believe that the other person's opinion is irrelevant.
And then the woman whose mother in law said she wanted to be there for the birth.
Right? So well, the concern here is that if she's going to be at the birth, then she's going to be heavily involved, and she is a narcissist, and makes everything about herself. So that is going to be difficult to deal with.
She won't be at the birth, not in the room, but she wants to be there, I'm guessing in the waiting room. I mean, that's not uncommon for the grandmother of the baby. This is not an uncommon situation. I guess it's really problematic. I don't know, it must be an issue if they don't want her there. Oh, mainly because I think stay with them get exactly right, if she's concerned about what happens before and after. And you know, and then she's going to maybe control the naming of the baby because you can't name the baby, something that she can't pronounce. And she obviously believes her mother in law is a narcissist. And that is going to be problematic in many ways. So having her at the birth at her most intimate time, her most intimate experience in her life, is maybe going to make her feel uncomfortable, whether she's in the room or not. If you have been listening to us or if you have taken our fourth trimester workshop, you know that we tell you to regard those first two weeks like life depends on it, because your postpartum recovery and your bonding with your baby and your breastfeeding success do depend on it. So if you don't want her there in the first two weeks, it is going to be important to set that boundary and to say, this is what we have decided and she probably won't like it.
Alright, the next one says, Hey, ladies, I'm a first time mom 26 weeks pregnant, doing a lot of research on unmedicated labor and birth in your podcast has been extremely helpful. I have two questions First, everyone always talks about tearing and getting stitches. But I'm wondering how that works in an unmedicated birth. Do they numb you before stitching you up? Or is that unmedicated to Oh, that's interesting.
She thinks good question.
She thinks one gets hell bent on the unmedicated thing. And then the doctor is like you said you didn't want medication? Did you? Without it now, we don't have to label these things. I think that's part of her her questioning here. Second question. What are your opinions for monitoring both mom and baby if you want a birth with free movement around the room? To me, we even have to ask that thing like like, what are your lights the option to move around? Don't say can we just say? Can I have the choice to move around, please? It's crazy. Yeah. All right.
All right. Well, okay. First of all, if you tear you don't necessarily have to be stitched many first degree and secondary degree tears do not need stitches,
and are better without them often, they heal better, right?
Yes, they Yes, because it's less damage to the tissue or you think about it at your perineum, tears. But then if you go in there and start putting a needle in four or five times, you're just putting more breaks in the skin. So in the midwifery world and probably in the obstetric worlds, it's common to say that if you put two sides of the vagina in the same room, they will find their way back to each other. And they really do. So they heal very well. So if you shouldn't need stitches, absolutely. You can have medication. Sometimes women don't because the tissue was so sort of numb after birth. But I would say the vast majority of the time, women do get some local lidocaine before they get the stitches.
But I wonder if she's asking because she wants, I feel like she's a perfectionist, perhaps and she wants to know if she can fairly and honestly say afterwards, she had an unmedicated birth. Don't worry about it. Yes, you can, by the way, if you Yeah, yes. And I don't think local medication really counts as medication and the birth is over by then anyway, but don't worry about it. Don't worry about the label or just look for focus on a comfortable satisfying birth. It's on your terms, do it on your terms. Don't worry about how others might label it and what the proper definition is. But I personally for what it's worth, I would say that still totally would qualify as natural birth if you 100% if your baby comes out without anesthesia. I mean, if that's your choice, why represent, you're not medicating the birth, you're, you're giving local medication to an injury. So we didn't answer the second part about the options for monitoring both mom and baby with the movement around the room and in different positions. So this is one of the downsides of continuous electronic fetal monitoring is that no, you can't move freely around the room, you are hooked up to a monitor, and you can only go so far as the monitor will let you go. But there is something called telemetry. And that is a portable, continuous fetal monitor. And then there's also intermittent auscultation, which is a whole separate discussion, but really what we want everybody the way we want everybody to be monitored birth, which means we just temporarily listen to the baby. And we're not hooked up to anything. And we have absolute freedom to move around the room and be in different positions without any restriction.
And for more information about intermittent auscultation, we have midwife, author, Amy Romano, who did episode 75 with us in January of 2021. It's called fetal monitoring and fetal distress. And it is a really information intensive episode if you want to learn all about the safest and the optimal ways to get heart rate so that yes, the takeaway is intermittent auscultation is preferable to continuous monitoring for sure. Okay, next question. Hi, ladies. This is how she's not That's how she started. She wrote Hi, ladies exclamation point. Then she wrote a one word sentence. Period. Okay. It's kind of how news anchor talks. They're like, got it.
I got it. I got it. Okay. Hi, ladies, exclamation point. meconium. Period. A friend of mine had her first baby 10 years ago. And the story goes that he was in the NICU due to meconium aspiration. And thank goodness, we didn't have a home birth because you would have died without immediate intervention. This tale is told to our community and scares many people, including my husband away from having a baby anywhere other than the hospital. What causes meconium aspiration? Is it preventable? Although the likelihood may be small, could it mean the difference between life and death at a Humber or a birthing center? Thank you so much for all that you do. I have been binging your podcasts as I look forward to my second birth coming up this October. Excellent question. Yes, it's a good one. So let's start with what is meconium. meconium is your baby's first stool, it's their it's the thing. That's the stuff that lines their digestive tract in utero. And sometimes babies have their first stool in utero, in labor, it happens, it's normal. But if it's too much, or the concentration of it is too high, because there's too little amniotic fluid, maybe your bag of water has been ruptured. For too long, maybe you actually truly had low amniotic fluid. If they're in the that, in combination with too much meconium can put your baby at risk for inhaling meconium. And that can get into your lungs, and it is extremely irritating to the lungs and dangerous and damaging to the lungs. Most of the time, if it doesn't get too far down in the lungs, it can it's not harmful. Or if it's diluted enough, it's not harmful. Sometimes we have to suction meconium out of the baby after birth if they're having a little bit of trouble breathing. And that usually resolves that. But if it really gets deep down into the lung tissue, it's is dangerous and damaging to the lung tissue. And so that's called meconium aspiration syndrome. It's rare. Can you still have a baby at home with meconium? Absolutely, it happens and midwives are trained on how to manage meconium. At birth, they they are trained in neonatal resuscitation, they have suction devices in case baby needs to be suction for an ammonium. They have, you know positive airway pressure for babies, the only thing that they don't have is the ability to intubate a baby. And that is the difference between something that could happen at the hospital that would be harmful to the baby. And the timeframe from getting a baby out of the birthing room and to be intubated at the hospital is much faster if you have a homebirth midwives are not trained to into intubate babies, they would have to call the EMTs and the baby would have to make a hospital transfer. But that is an unusual scenario where you would actually need to intubate a baby. I've only heard of sectioning and all the that's most of the time. Yes, that's most of the time what happens. The only time you didn't need to intubate is if a baby truly wasn't able to use their own lungs and you had to create artificial, you know, to help them breathe. I've seen one time a baby who actually had meconium aspiration syndrome. So they had the most extreme severe case of it. They were born at home. We had suction we had oxygen we call the EMTs. The baby made a hospital transfer and it was managed at the hospital.
All right, I think it's time for quickies. All right.
Let's do it. Here we go. First one. Is it normal to still be able to express some milk for my breast 10 months after stopping breastfeeding? Yes, it is. You might even up to a year I've seen women still be able to express milk, tiny tiny bits for talking drops. But yes, it's normal.
Is VBAC homebirth a safe option, also known as h back home birth after cesarean? Well, we know it has a much higher success rate than the hospital.
I mean, yeah, I've talked about this, I think what episode was it in November of 2020. We talked about it was our V back special. And I've had so many clients have successful V backs and over the years, it's been over 95%. More than half for homebirths.
They're more successful than a V back at the hospital or talech at the hospital.
Yeah, so it's safe. It's up to the homebirth midwife as to whether you need to be risked out for some other reason. But of course, it's safe your body only knows one way to give birth. And while you might be hearing about the risk of uterine rupture at every turn, it's only a little bit higher than the risk of uterine rupture for first time mom who never ever ever hears about uterine rupture. So VBAC moms are carrying this heavy weight with something that is only a little bit statistically more likely to occur for them than a first time mom in the first place. But it's really for you and your home birth midwife to decide, but the answer is definitely yes. And my mentor is a really a world famous author and midwife named Nancy Waner, published under Nancy Waner, Cullen, and she is a home birth midwife specializing and be back and she's attended almost 3000 births, and some of those women had four C sections before their fifth birth vaginally. That doesn't mean it's right for you. It does definitely point to its safety. Statistically speaking. Does anyone ever Sue and I'll be looking at this one for a psychological damage. And when I hope so, wow, that's really interesting. You know, who we need to ask, obviously, or mean? Or mean? Who does an EP who has done a couple of episodes with us already? There's a third one coming out in I believe it's coming out in June, and attorney defending women's rights in hospitals. If you didn't catch our first episode with her it was in early December 2021. And then last month, we had our second episode with her. I don't know we'll have to ask her this, Trisha.
I'm sure it's a hard case. I'm sure it's happened. I'm sure it's a tough case to win. But we're, it should happen more often. We know that it's a tough case to win. Because first of all, there's a bias toward medical providers from everything we've garnered from her mean over this time, but primarily because you'd have to prove psychological damage. And then you would have to prove that damages are owed for it. For example, the psychological damage was so severe that you weren't able to work. So those would be the damages. We don't know. If we get any information, we'll share it. I'm very sorry that anyone is honestly, I'm very sorry. Anyone who's asking this question, because you know, they've been very hurt. I'm sure there are fantasies about going to court and telling everyone, whatever happened to them?
Totally. I mean, 1/3 of women experience birth trauma, you know, looking that provider in the eye and making them understand the suffering. That would be satisfying, even if no financial damages were sought.
When we're talking about emotional trauma. When we're talking about birth trauma, a third of women experienced emotional birth trauma, truly unbelievable.
Next one, would it be a bad idea to add dates to my smoothie at 35? Weeks?
No, of course not. It'd be a good idea.
She's asking this because she's concerned that too many dates too soon could put you into preterm labor. But no, no, it's no not yet. You can definitely put dates in your smoothie. The recommended amount to get your cervix ripened and ready for birth is six dates per day.
From what point on isn't like 38 weeks, I think it's 36. Yeah, so but you can actually, you know, go ahead put a few dates in your smoothie because it makes it sweeter, but you're probably not gonna put six or eight dates in because that would make it twos to sweet.
Well, maybe not. I've had them not date smoothies with raw cacao that are I'm thinking I might have had that many in there. Maybe maybe but you know, I think the the read the thing she can probably feel good hearing is, even if it were like extraordinarily effective. it ripens the cervix, but that's only the very early part of labor beginning the surge is actually have to begin the contractions actually have to begin that's with the release of oxytocin. I mean, that has to get the uterine in the uterus in action. And the dates don't do that. They just soften the cervix in the way that prostaglandin does.
I mean, we wouldn't need Pitocin if they worked out well, so
All right, I had his tips to help keep milk supply up while sick. Is that a quickie? Um,
I don't know. That's a quickie, but I guess we could suffice it to say that definitely your milk supply can go down when you're sick, it usually rebounds pretty well, after hydration is going to be key. nursing your baby is going to be key. But it's normal to expect that your supplies going to go down a little bit. And when you recover, it should also recover.
What's the what's the number one thing to do to ensure baby is in a good position for birth?
The number one thing can we think of the absolute number one thing, I would say remain more forward leaning than reclined in the last weeks of pregnancy. Because you want the back of the baby's head, which is the heavy part of the skull to rotate forward. If you're leaning back all the time, it's more inclined to rotate backwards.
Right? If you were It's a strange visual, but it's helpful but I've seen a doula demonstrated this way where like if you kind of had like if you held a pencil right in front of your your navel and it were sticking straight out perpendicular to your body, if that pencil is tipping downward to toward the floor that's optimal, as opposed to tipping upward toward the ceiling. Yes. I have a relative who has previously had two C sections for both Herbert's due to amnio low amniotic fluid. Boy, do I have questions there, right. She wants to do a VBAC, but the previous hospital is declining her this course and in the state of Florida, you cannot go to a birthing center for a VBAC at this point. Wow. That's a disappointment. I did not know that.
She could still go to the hospital. She wants to do a VBAC. But the previous hospitals, oh, previous hospitals are declining her and in the state of Florida, you can't go to a birthing center, either find a different hospital that will do a trial of labor after cesarean or have a home birth or go out of state. Those are the three options.
Research shows feedbacks are statistically consistently safer than repeat cesarean sections. It is so disappointing that women end up in this situation. And you know, I made reference to how many clients of mine had homebirth VBACs. It wasn't that they wanted to it wasn't that that was their first choice. They were driven to it because they became increasingly committed to the idea of a vaginal birth. And they ran out of options. Anyway. It's disappointing. Not evidence based should not support VBAC.
Absolutely. Does having an anterior placenta affect your labor experience at all? If so, is there anything that can be done to prepare for birth? So there's nothing you can do about having an anterior placenta once you have it? That's for sure. And does it affect your labor experience? Not really, it might affect your ability to monitor the baby. Sometimes, that can make it a little bit more challenging. And sometimes it can change the placental delivery a little bit, just the way the placenta separates, if it's in the anterior position, but I don't think you need to concern yourself with this. It's like just kind of forget that you have an anterior placenta, don't worry that it's going to do anything differently in your labor. And now there isn't anything that you need to do to prepare for birth with an anterior placenta.
I did for my second birth. You did what? I had an anterior placenta and I remember going oh my gosh, what does that mean? What does that mean? Yeah, Nancy, the mentor I just made mention of was like, it means nothing, nothing. Now, I was like, what, what? No, it means nothing. And she said, I don't remember anymore. But she said something like it's did she say 20% of births or something? It's really like half a percent. Now. It's just like, you're rare. It's not a percent that attaches. Yeah, it's I mean, maybe you you all have to remember nature has you covered. Nature does not need all the stars to perfectly aligned for a wonderful safe birth. Nature is prepared for all the variations but adaptations. Yes, yes. That's why things like molding happens. That's why the pelvis opens up. I mean, you don't have to expect everything to be a certain way. But that is the message you get from our medical community. But it's not how nature sees this at all. You're this is really an anterior placenta is. It's kind of a non issue. It's that common. Yes.
Great. All right, last Quickie, I'm 10 months postpartum, and I'm experiencing huge mood swings and weakness out of the blue. It I feel like I'm back in the baby blues is this normal?
Oh gosh. Well, it's unfortunate that that's happening. So postpartum depression, postpartum anxiety, any perinatal mood and anxiety disorder like postpartum rage, any of the above, it can begin anytime in the first 12 months. So because our community and our loved ones and our society isn't informed, it's really scary when that happens 10 months out, often when this happens is because of a trigger. So the first myth is that it's linked to hormones. It's not linked to hormones, but often when it happens far out. It's a trigger. It's the change a move your partner goes from working at home to working in the City Year. You know, get the A good friend moves away, there's a divorce in the family, your pet dies, there's often a trigger when it happens. So do take this seriously, and join a support group, maybe look into getting clinical help. We should mention, Trisha, we don't mention enough all the work we do is online and we serve our podcast listeners as much as you know, they're our clients too. So if you're ever interested in being in our Postpartum Support Group, our fourth trimester workshop Trisha is breastfeeding workshop my HypnoBirthing classes contact us that's a good percentage of the community that we're serving now. All right, everyone, thank you so much for your questions. And if you find this podcast valuable, beneficial entertaining enjoyable in any way and you know anyone who might benefit from it, please share it with them, tell them about us, send them an episode. And and join us over on Instagram if you want to reach out think about this 1000s of people listening to this episode, if everyone just shared one episode with one person, how that would expand our reach. That would be awesome. So if you have a moment, we'd love for you to do that.
Not millions but more. Thank you everyone. We'll catch up with you next week.
Thank you for joining us at the Down To Birth Show. You can reach us @downtobirthshow on Instagram or email us at Contact@DownToBirthShow.com. All of Cynthia’s classes and Trisha’s breastfeeding services are offered live online, serving women and couples everywhere. Please remember this information is made available to you for educational and informational purposes only. It is in no way a substitute for medical advice. For our full disclaimer visit downtobirthshow.com/disclaimer. Thanks for tuning in, and as always, hear everyone and listen to yourself.
Recent Episodes
Subscribe
Between episodes, connect with us on Instagram @DownToBirthShow to see behind-the-scenes production clips and join the conversation by responding to our questions and polls related to pregnancy, childbirth and early motherhood.
You can reach us at Contact@DownToBirthShow.com or call (802) 438-3696 (802-GET-DOWN).
To join our monthly newsletter, text “downtobirth” to 22828.
We'd love to hear your story.
Please fill out the form if you are interested in being on the show.
Subscribe to The Show
Follow Us On Social